去YMCA take了周末两天的急救certification课.
这篇文章是纯笔记,会新开一篇简单谈谈感想!
顺便一提急救证书每三年要求重新考试与更新 - 因为急救的知识与标准一直在更变.
Rule 1 - 3P’s
- Preserve life
- Prevent future injury
- Promote recovery
Intro
First aiders:
Someone at an emergency scene who suspects injury or illness and responds by:
First aiders do not diagnose, or provide medical help -> that is hospital’s job.
What they do:
- taking charge of emergency scenes
- providing assistance to other rescuers
- reassure victims
Some companies formalize procedures for first aid response.
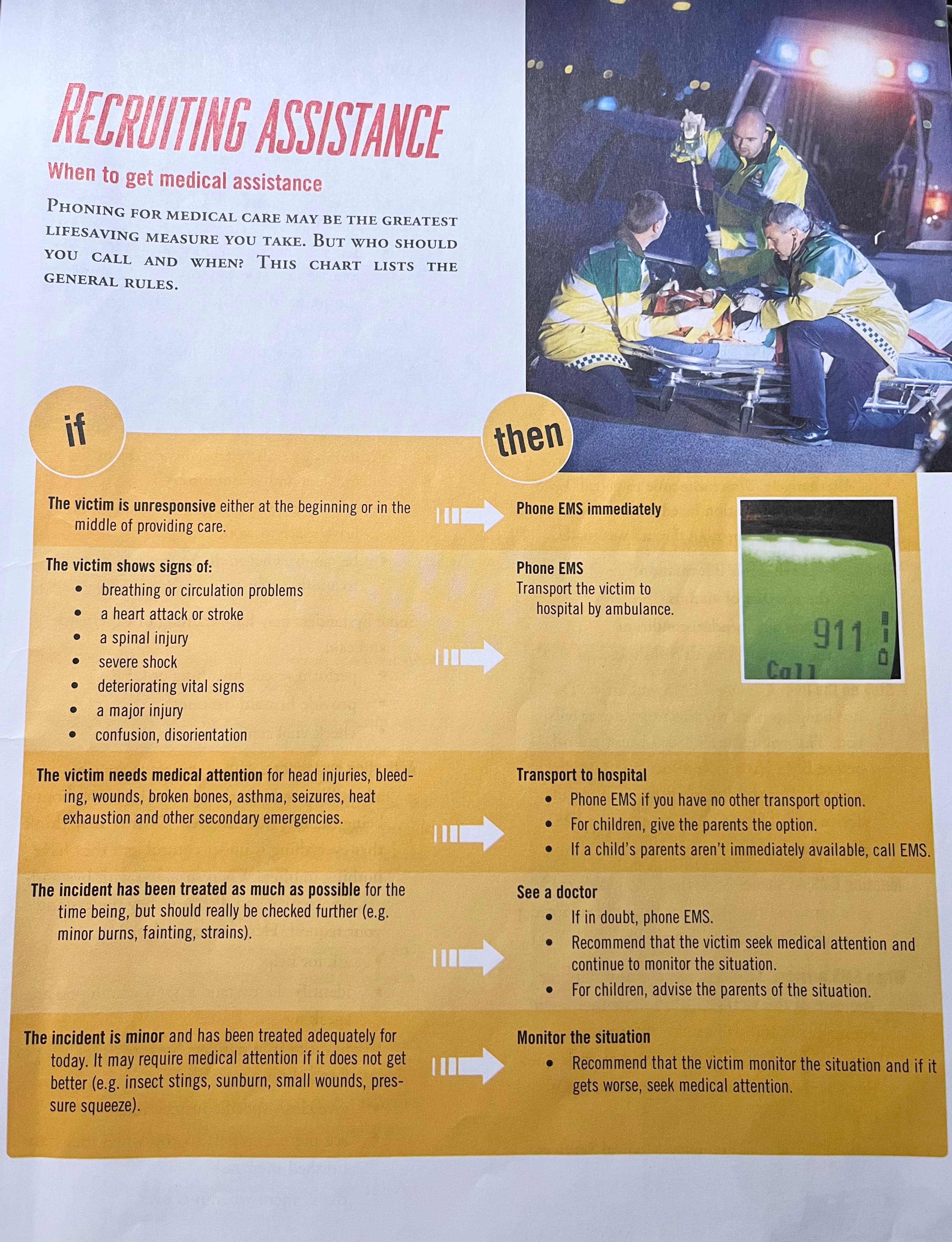
EMS: Emergency Medical system, consists of police, fire and ambulance.
Role as a first aider inn an emergency that requires medical help is to:
- active the system with a telephone call
- care for the victim while waiting
When call:
- the number of victims
- victim age, gender, condition
- the location where EMS should go
Stay on the line: ask when EMS will arrive. Do not hang up until the EMS dispatcher tells you. This will ensure the call is not cut off before before EMS has all the info needed to respond.
The law
When to start:
- gain permission if the victim is conscious -> can ask more times tho
- act reasonably within the scope of training
- continue until someone more qualified takes over unless you are at risk, or exhausted (or victim say i’m okay)
Get consent:
- if victim is unconscious (consent is assumed)
- if victim is minors (ask for parent/guardian < 16 or unaccompanied) -> if no parent then yes
Legislation:
Most provinces have an act that protect first aiders from liability for damages allegedly cause during first aid assistance (through a careless act or omission)
Such as Alberta’s emergency medical aid act or Ontario’s good samaritan act.
Standard of care:
If there are any questions about the level (or standard) of care you provided, the court asks the general questions, “what would a reasonable person with your training do under the same circumstances?” As long as you do what you were trained to do, you are protected by the law.
Do not resuscitate (DNR) orders:
A DNR order is a written formal statement communicating the person’s decision to decline resuscitation should they stop breathing. These orders may appear within other documents such as “advanced directives” or “living wills.”
DNR orders are rare in first aid situations. First aiders should proceed with CPR if required unless presented with a DNR order.
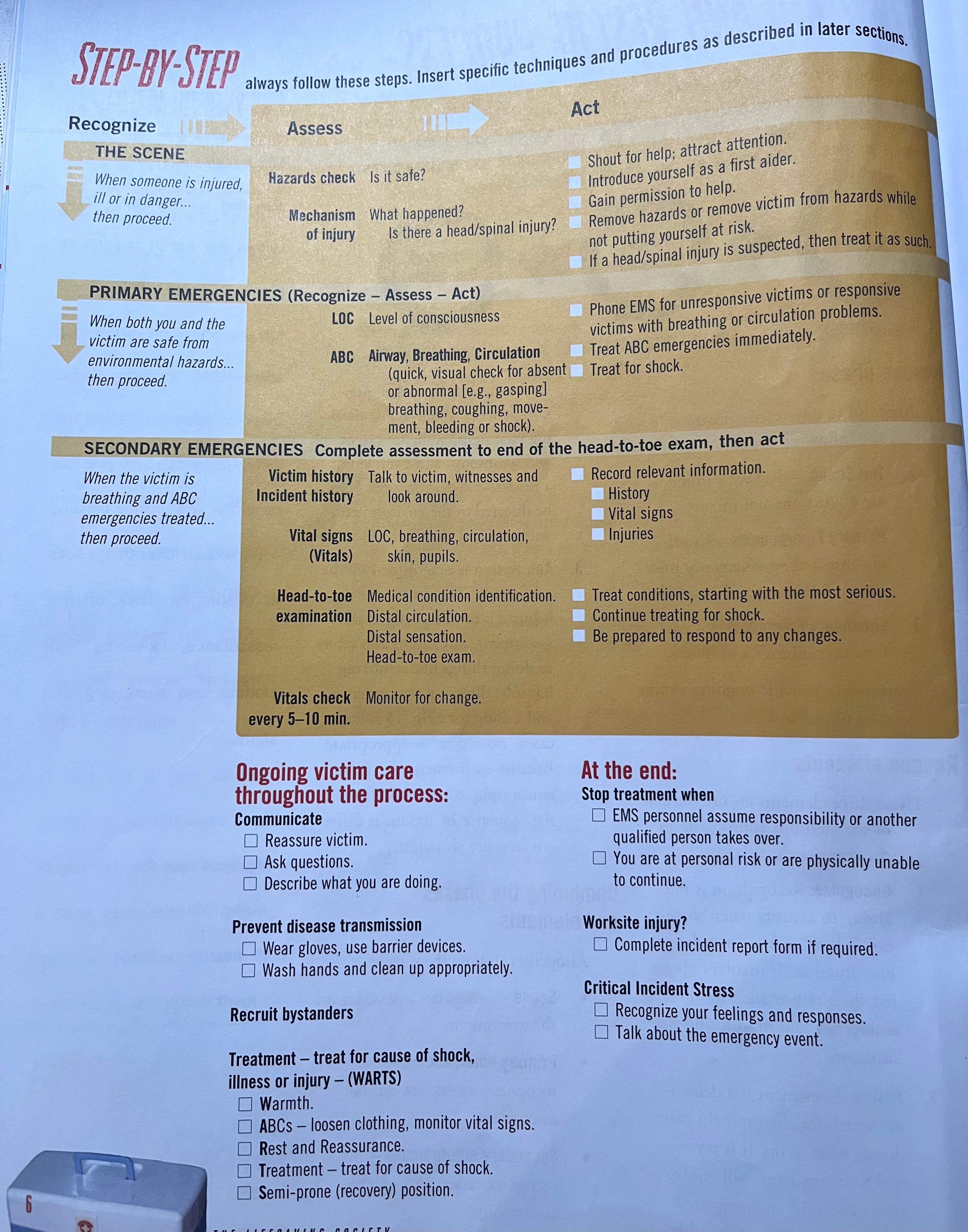
The Scene
Deal with immediate environmental threats.
Area check. Work around the victim.
Recognize:
recognition is the ability to identify when someone is hurt, sick, or in a dangerous situation. It involves observing the circumstances of the emergency and monitoring the situation.
Mechanism of injury.
Assess:
assessment is a deliberate search for clues to help you decide what to do. It is pivotal to first aid and will guide your actions in an emergency.
Assessment can take a number of forms: look around, question or series of questions, checking vital signs, evaluating signs and symptoms, and completing a head-to-toe examinations.
Act:
determined by the assessment. The act of treating injuries is one response to the assessment. Some cases “no action” is appropriate.
If ask bystanders to help -> they do not need to be trained.
Crowd control can be one of the thing needs to do.
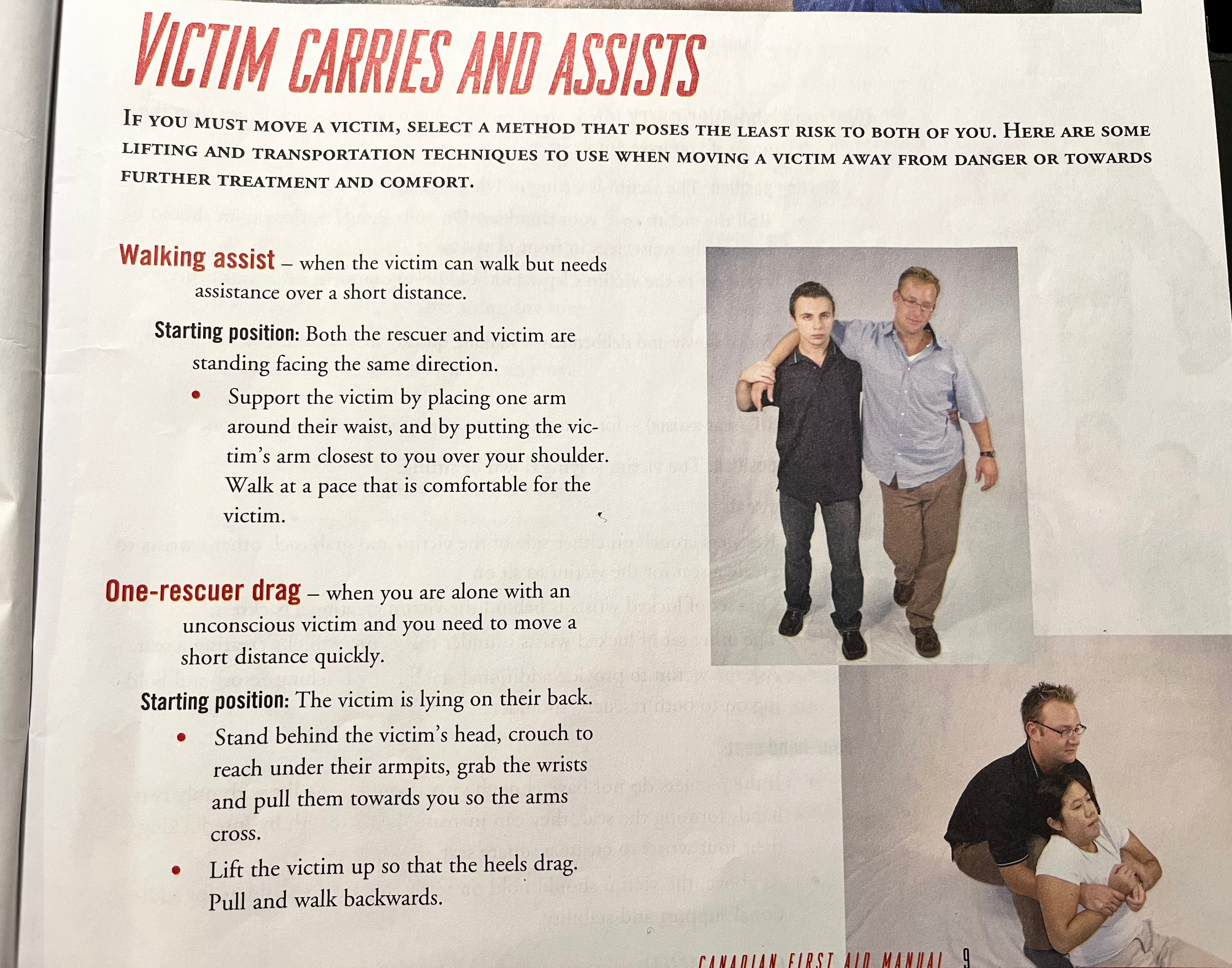
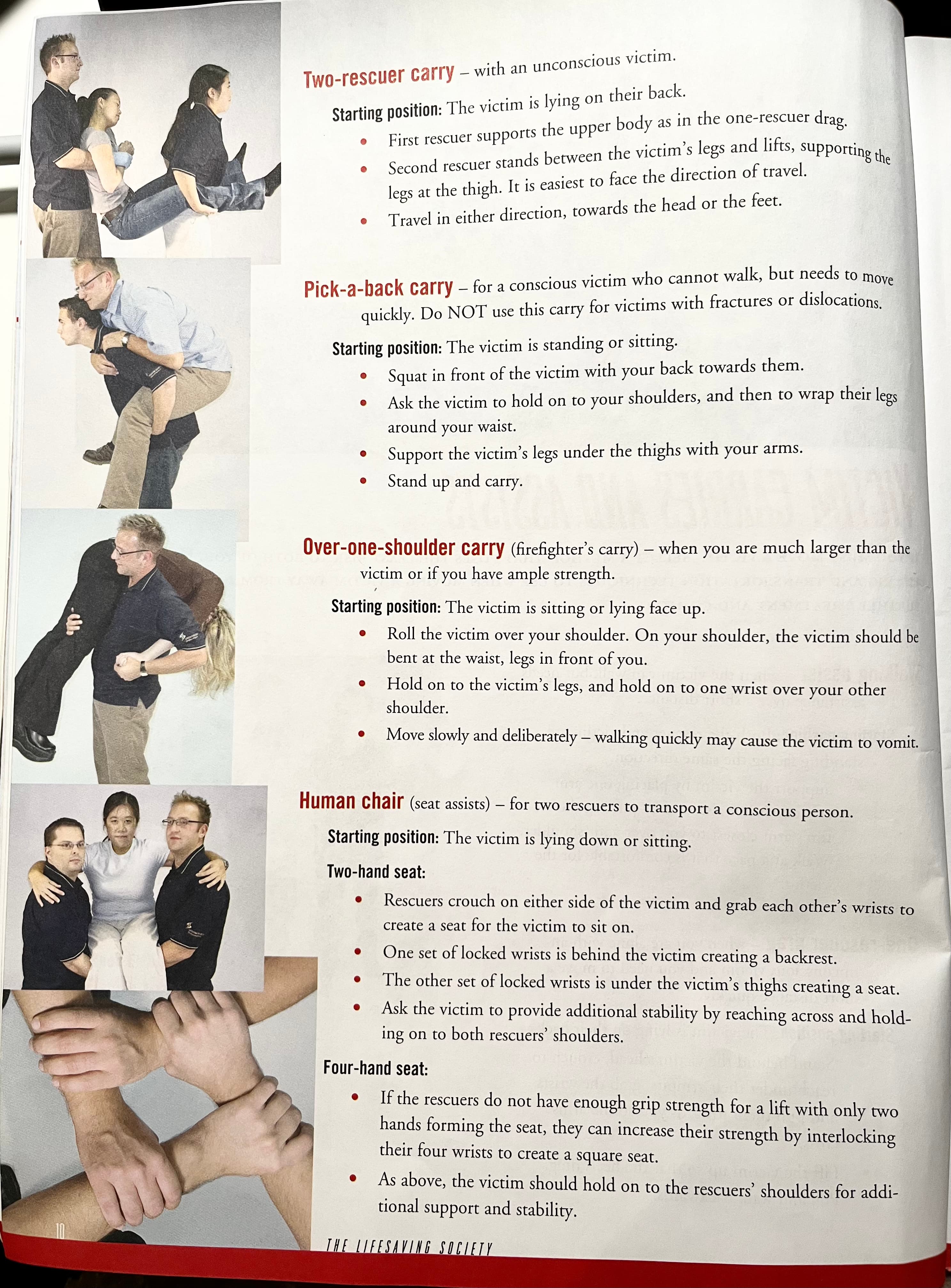
victim carries and assists
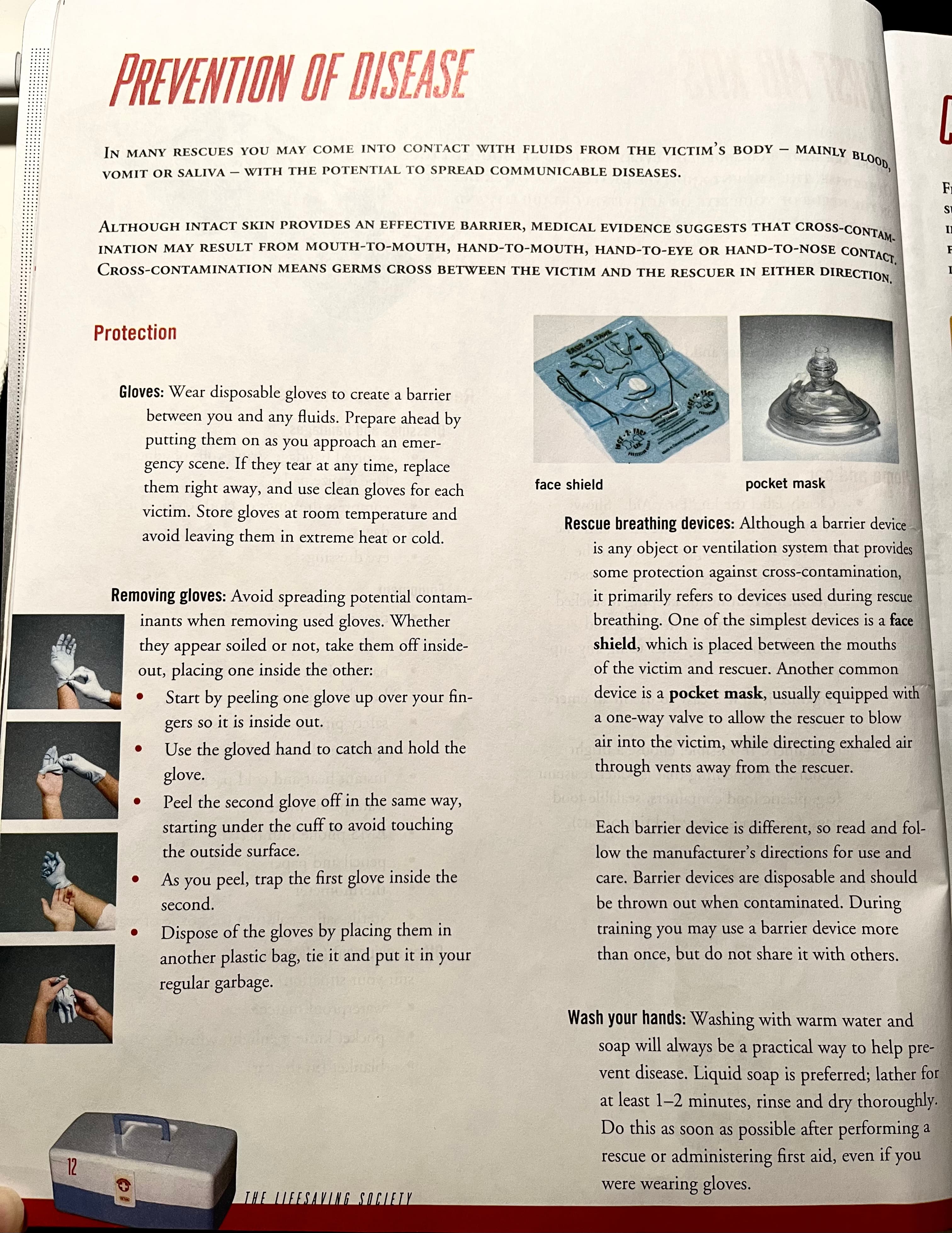
Personal protective equipment(PPE) -> protect both victim and first aiders.
- gloves
- masks and face shields (various types)
- gowns
- goggle
Recommended contents
- assorted bandage strips, rolls of adhesive tape, gauze pads
- compress dressings or cloth triangular bandages
- eye dressings
- tweezers, scissors
- safety pins (assorted sizes)
- splints and splint padding
- instant heat and cold packs
- waterproof waste bag
- pocket knife, penlight, whistle
- blanket (in the car)
Multiple victims:
When there is more than one victim, emphasis is placed on doing the most good for the greatest number. Therefore, treat victims with the most serious life-threatening injuries first, such as respiratory arrest or major bleeding.
First, conduct a primary assessment on all victims and immediately contact EMS if any victim is unresponsive or distressed. If you are treating multiple victims with life-threatening injuries, and cannot recruit enough help to treat them all, those with no sign of circulation are the lowest priority for treatment.
Proceed to secondary assessment only after you’ve dealt with the ABC priorities for all victims.
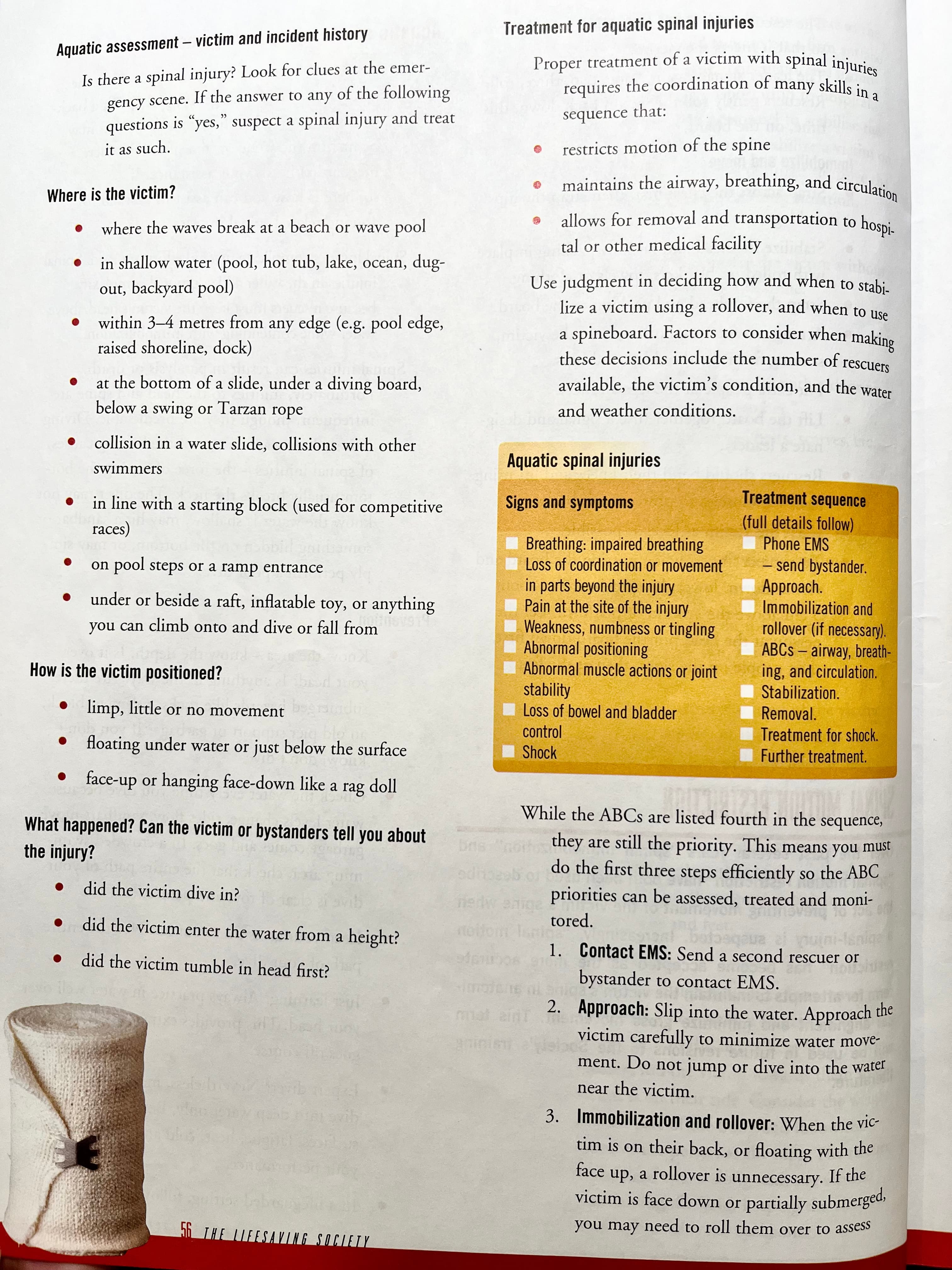
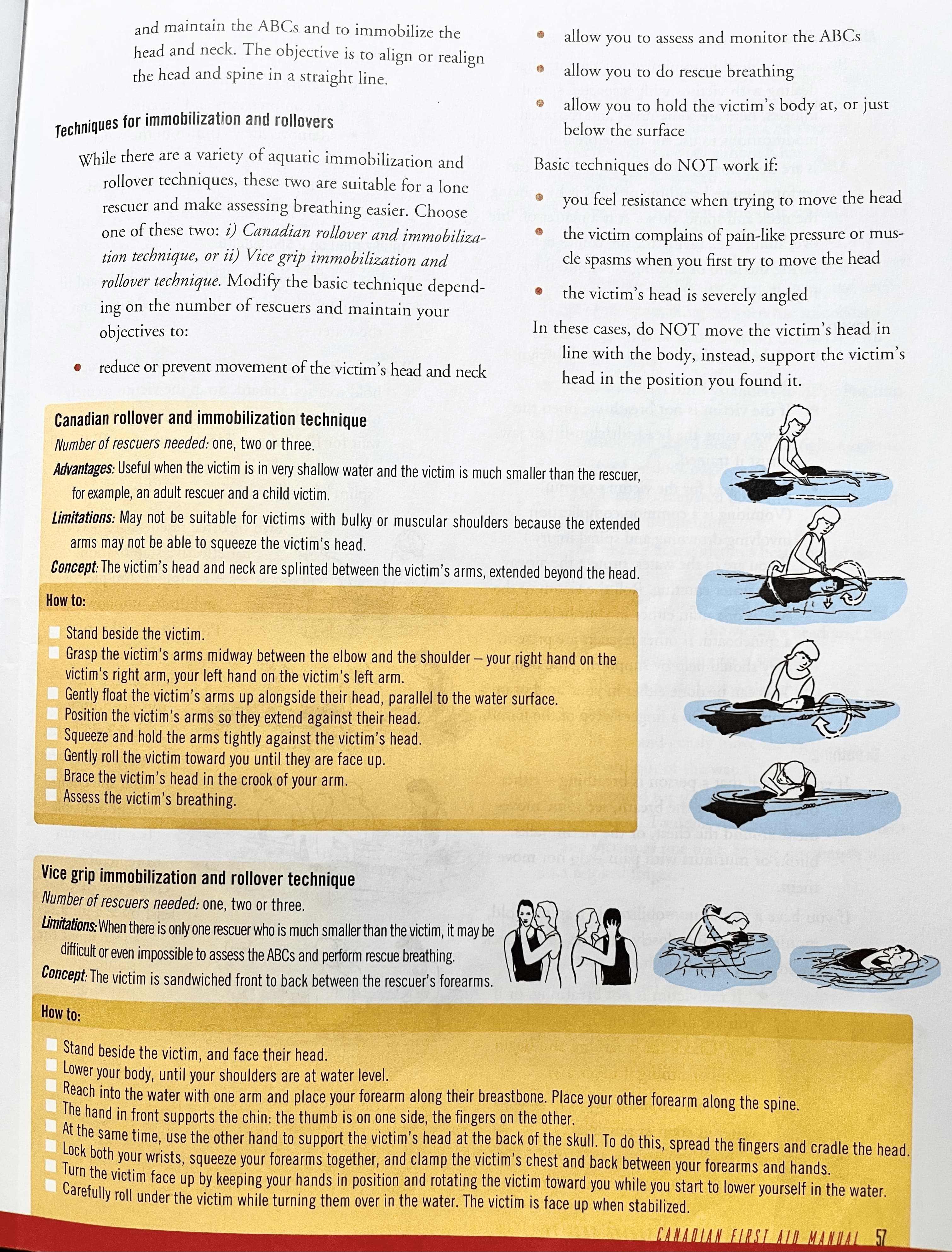
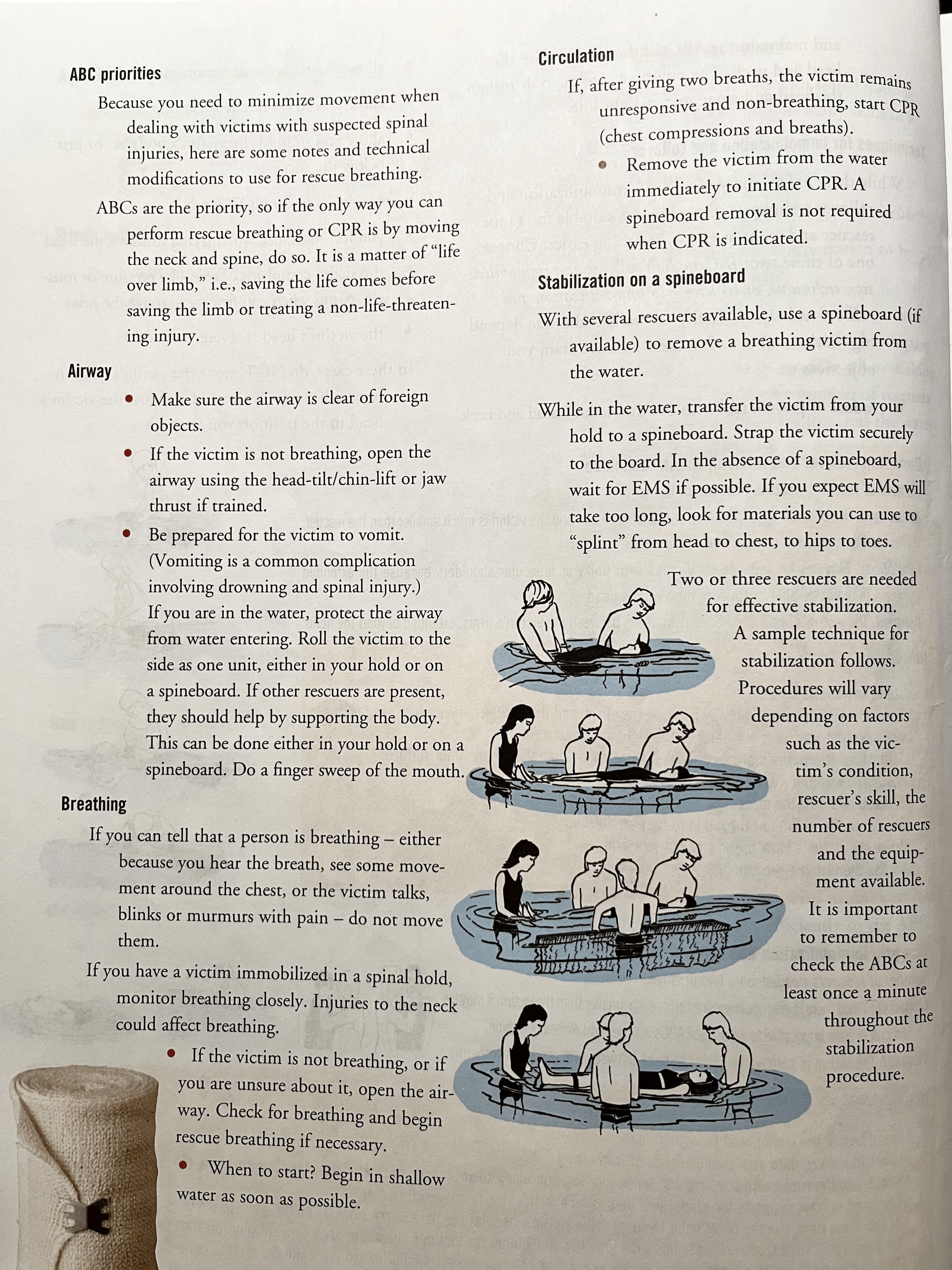
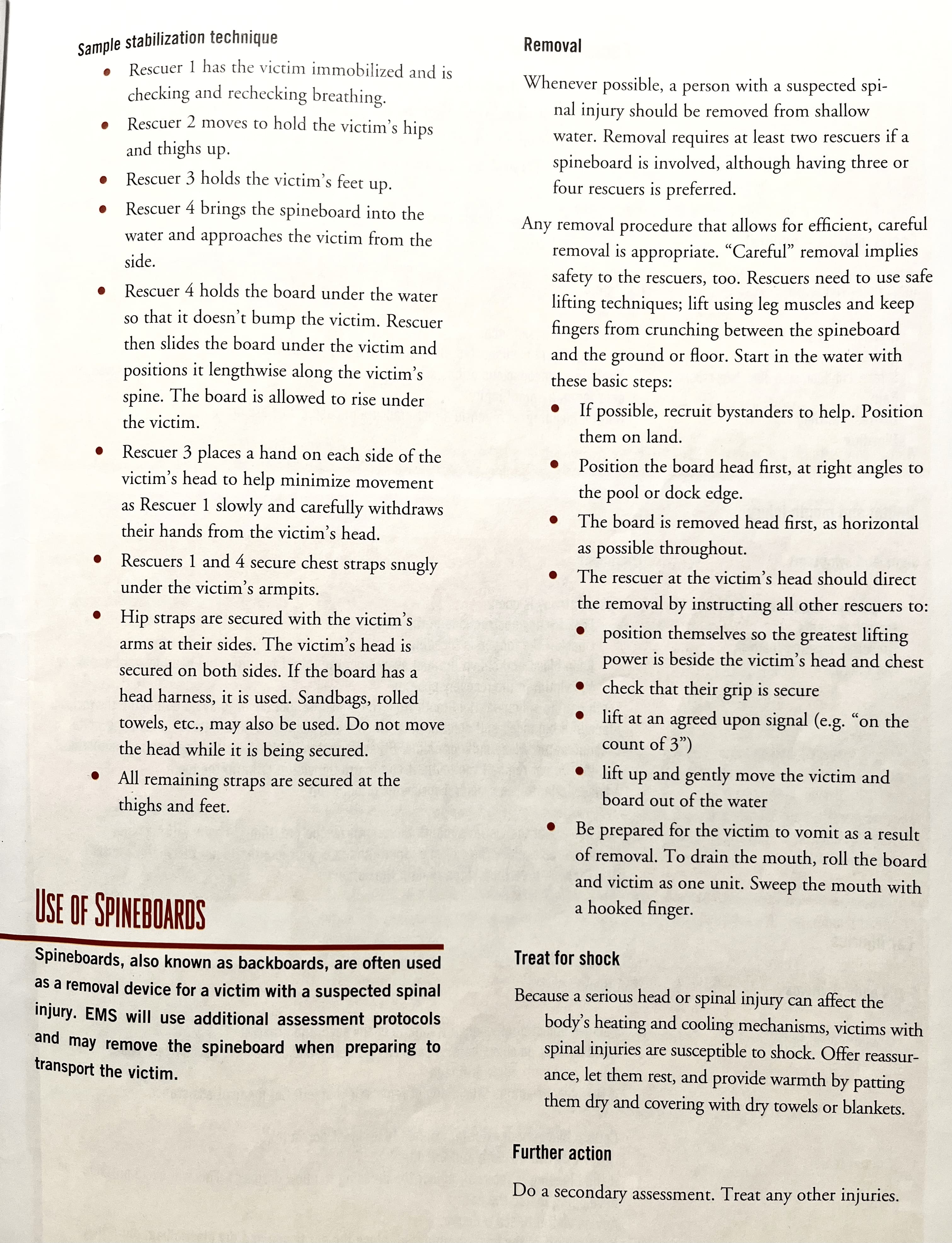
Spinal injuries:
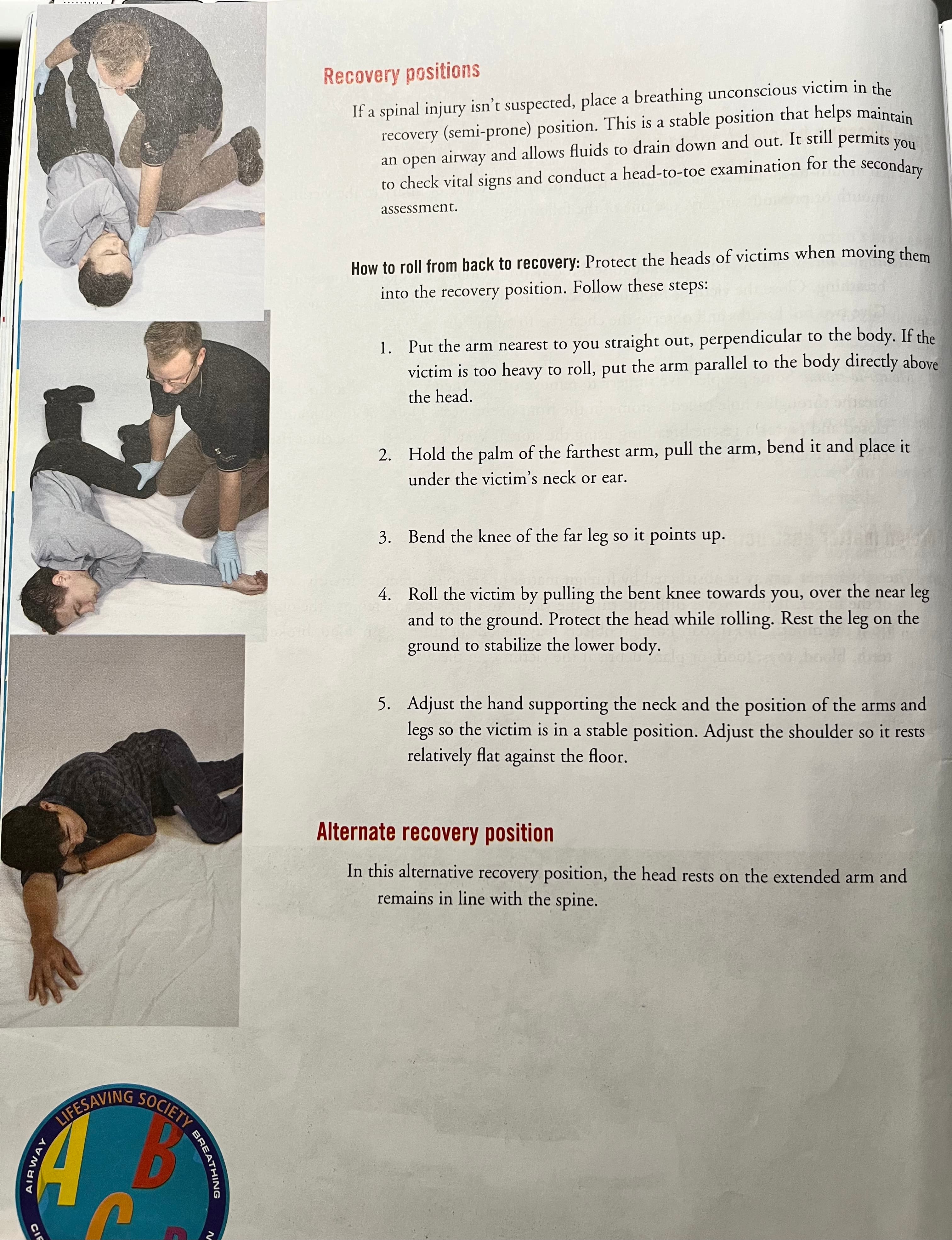
If you suspect a spinal injury, treat the victim as if there is a spinal injury. Do not move the victim (as far as conditions allow). Prevent movement by asking a bystander to hold the victim’s head and neck still. If you are alone, use available objects to support the position of the victim.
Preliminaries:
- Say “hello” and introduce yourself
- assure them of your skills and experience as a first aider
- ask if you can help - you must obtain the victim’s consent before continuing
- learn and use the victim’s name
- start reassuring victim immediately
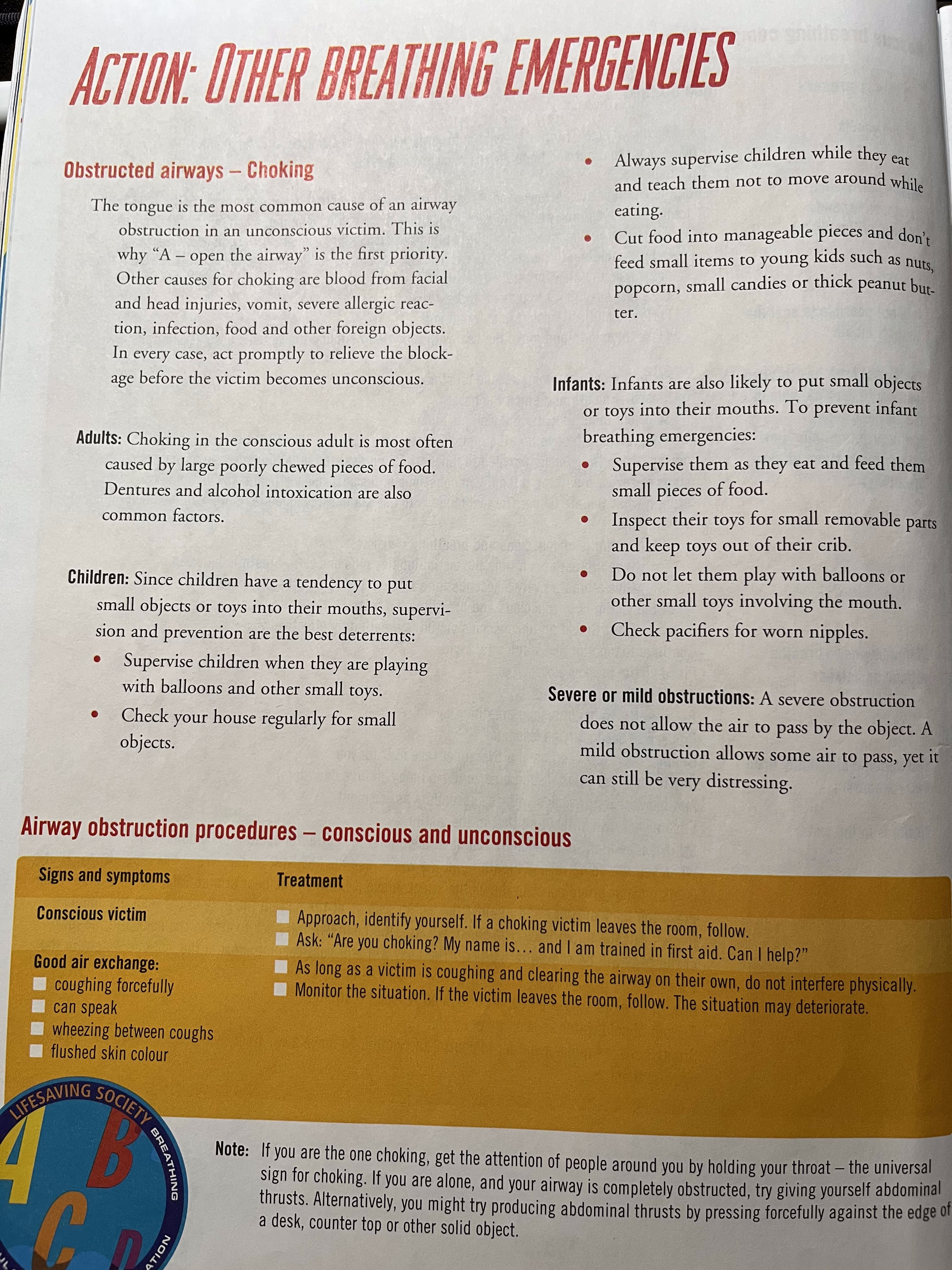
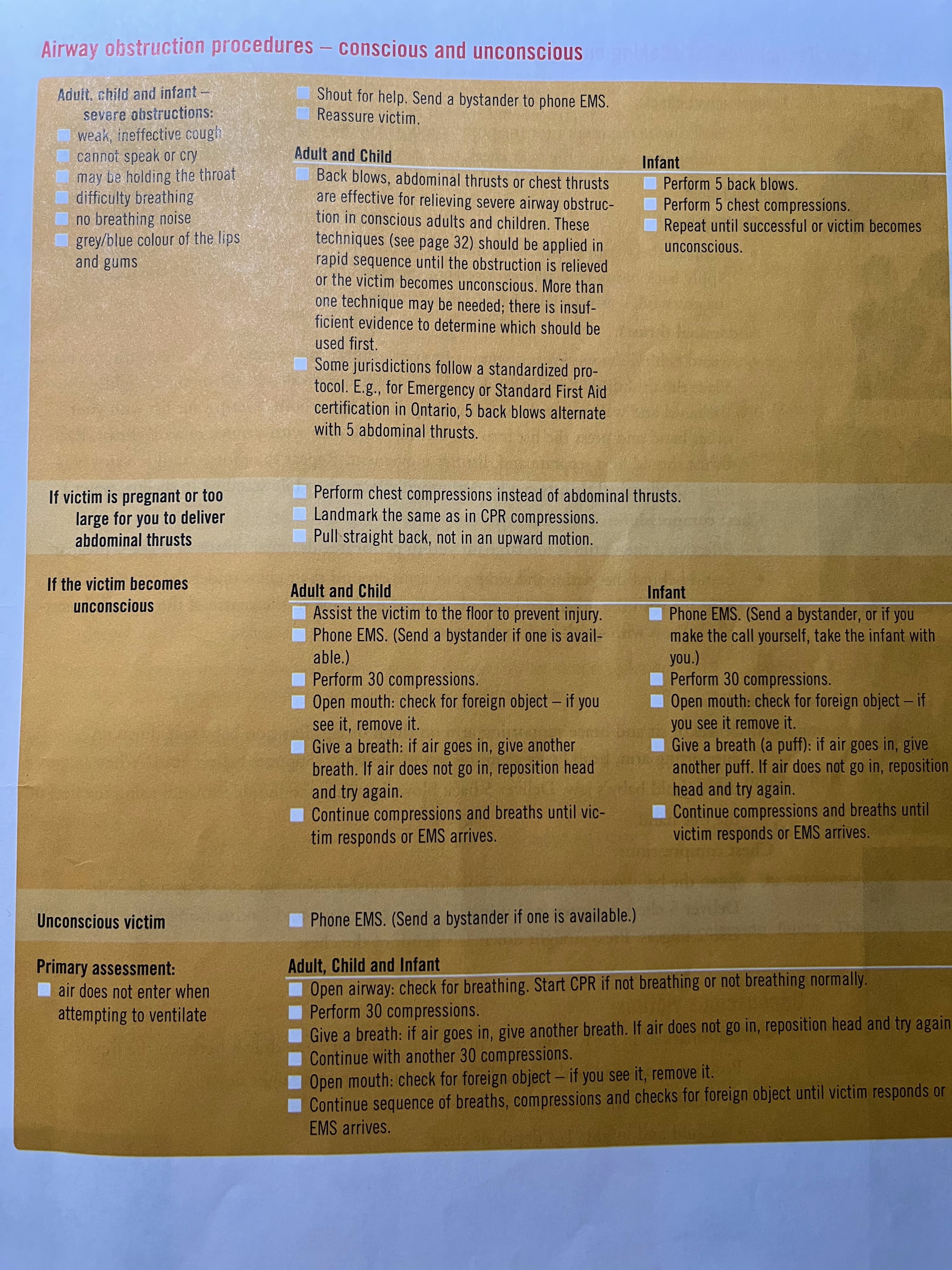
Primary Emergencies
Handle life-threatening emergency priorities of breathing and circulations.
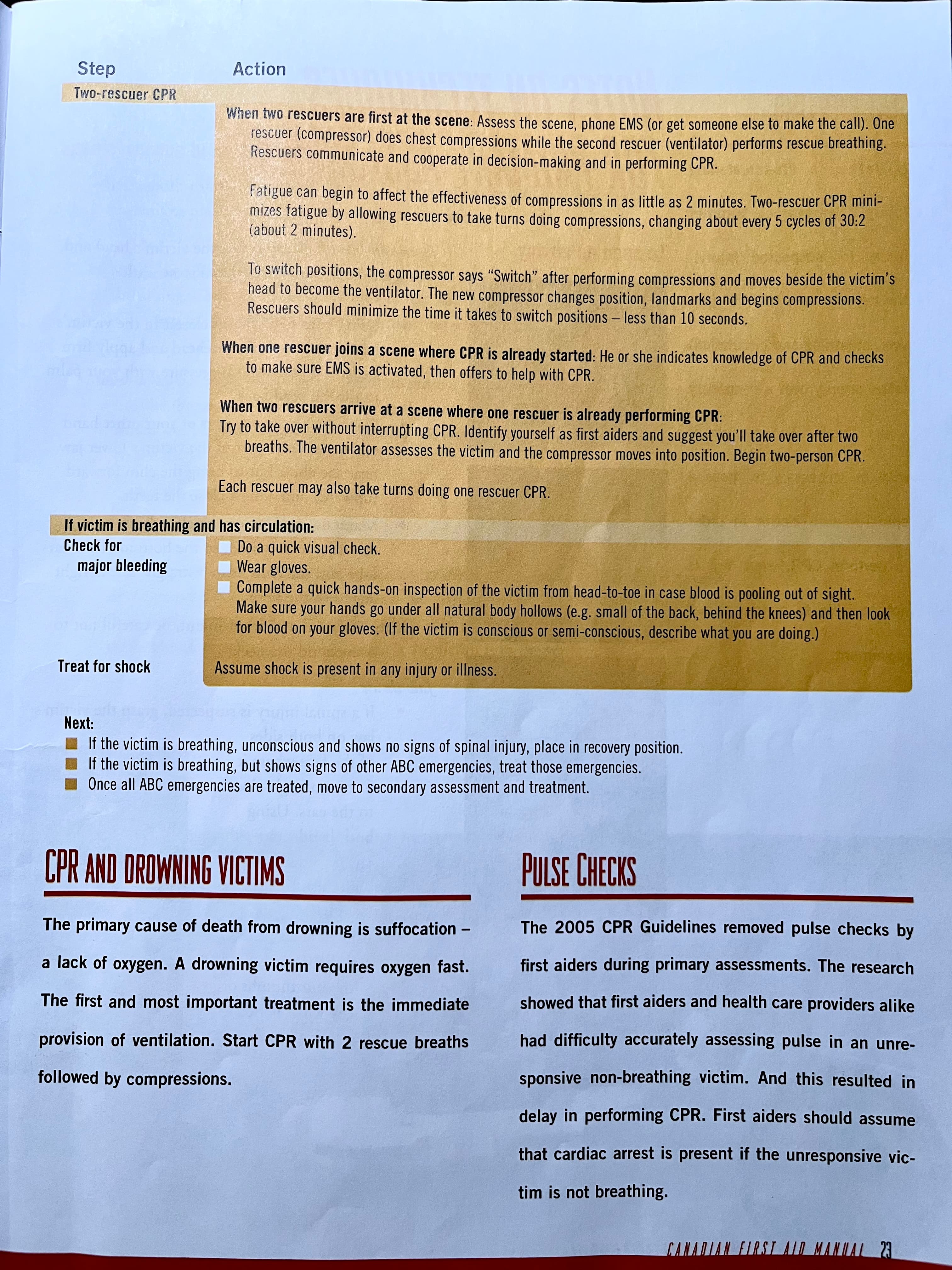
Airway(nose, moth, throat, trachea).
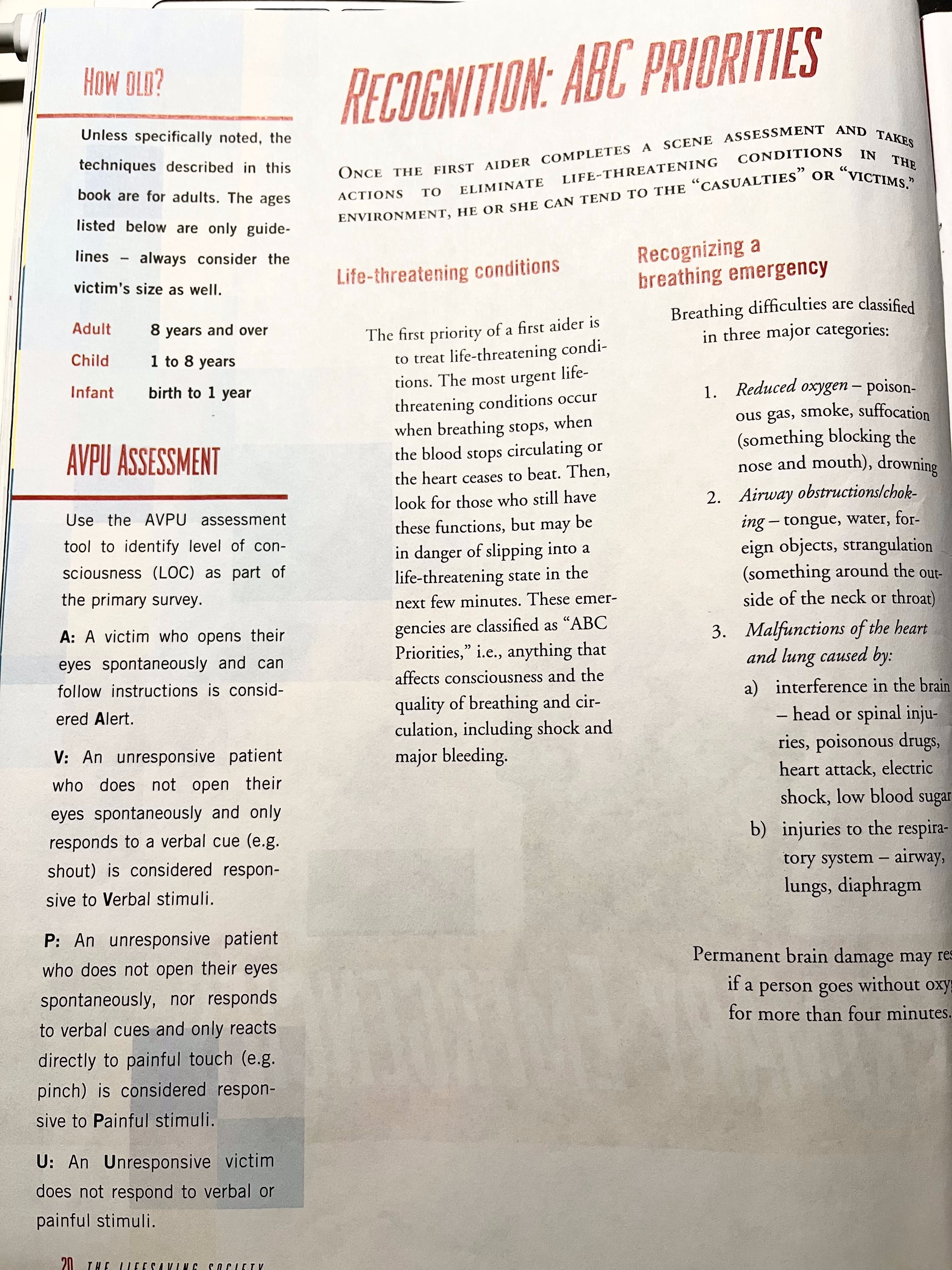
Breathing difficulties are classified in three major categories:
- Reduced oxygen - Poisonous gas, smoke, suffocation (something blocking the nose and mouth), drowning
- Airway obstructions/choking - tongue, water, foreign objects, strangulation (something around the outside of the neck or throat)
- Malfunctions of the heart and lung caused by -
a) Interference in the brain - head or spinal injuries, poisonous drugs, heart attack, electric shock, low blood sugar
b) Injuries to the respiratory system - airway, lungs, diaphragm
Permanent brain damage may result if a person goes without oxygen for more than four minutes.
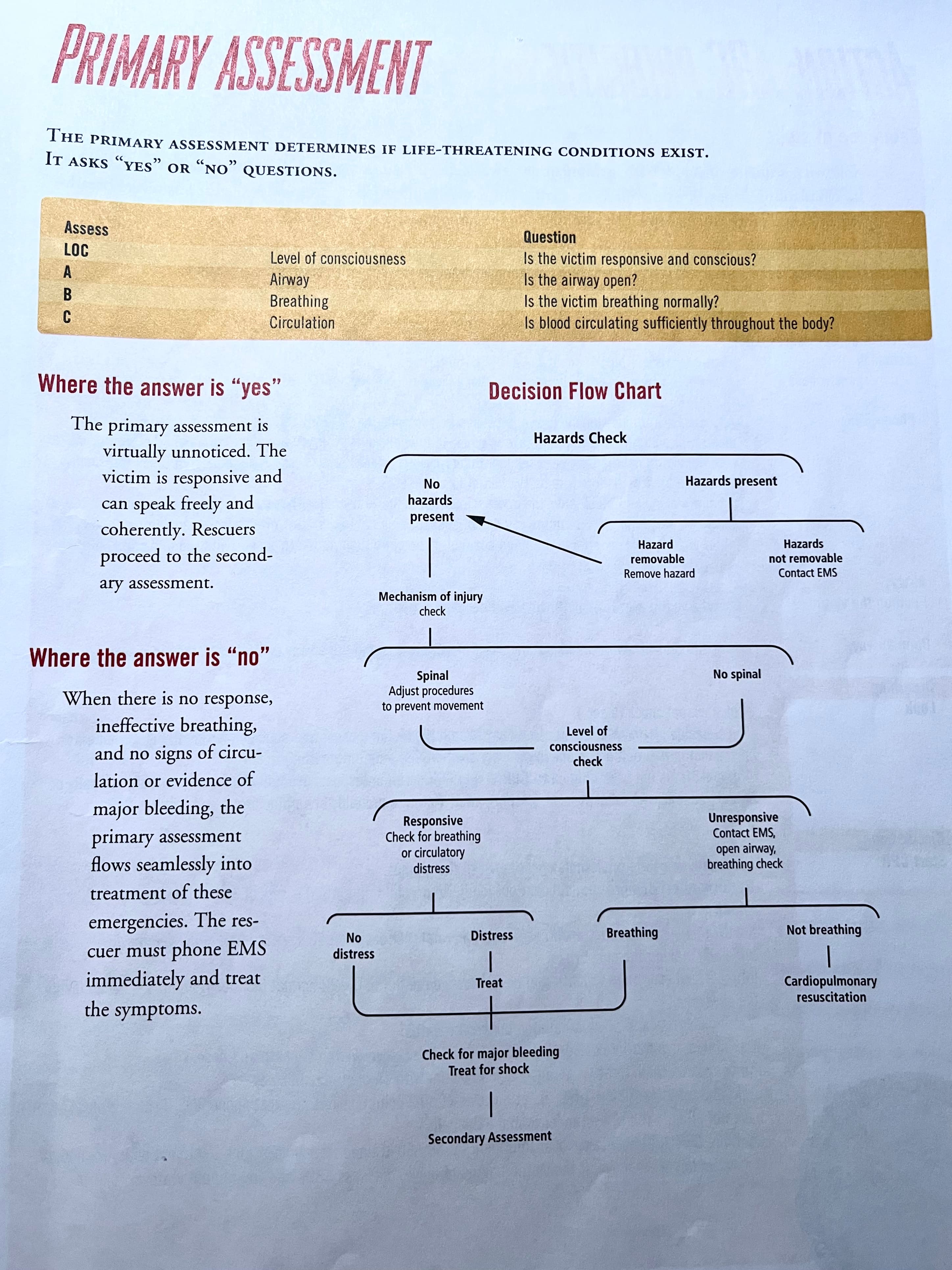
Primary assessment.
area check -> things may hurt victims
awareness -> level of consciousness, AVPU (alert, verb, pain response, unresponsive)
ambulance -> decide whether to call EMS, verb maybe, anytime to delay call EMS, that would cause the victim in risk, after call for bystanders, ask for them to come back, confirm EMS call
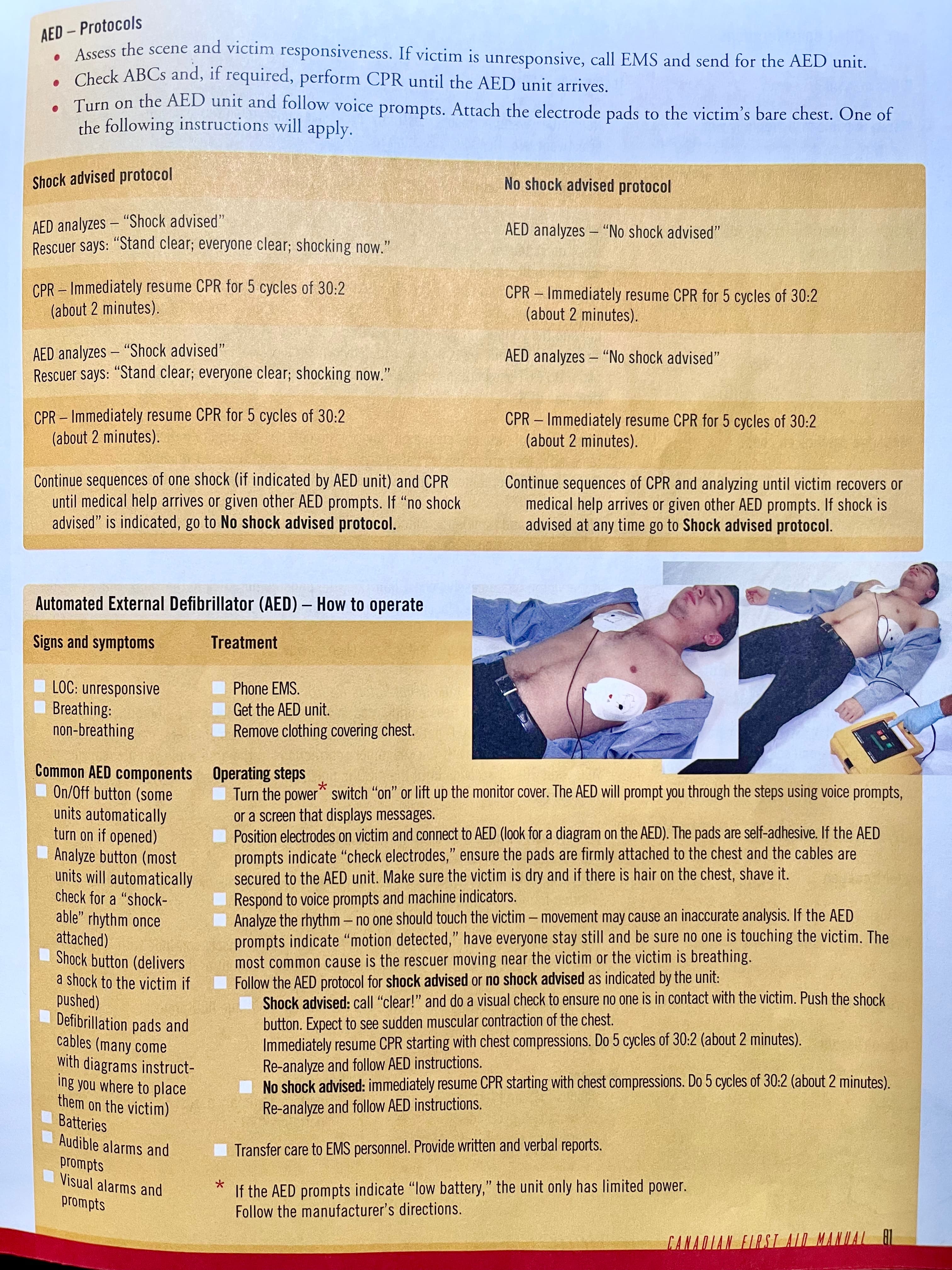
AED -> more successful than CPR
airway (eg. speak response)
breathing
if breathing, look for bleeding, check the heads, underneath the tortuous, check under arms, no major bleeding, recovery position -> unconscious and breathing (quick one instead of head to toe)
circulation (first aid don’t do pulse check) -> checking bleeding
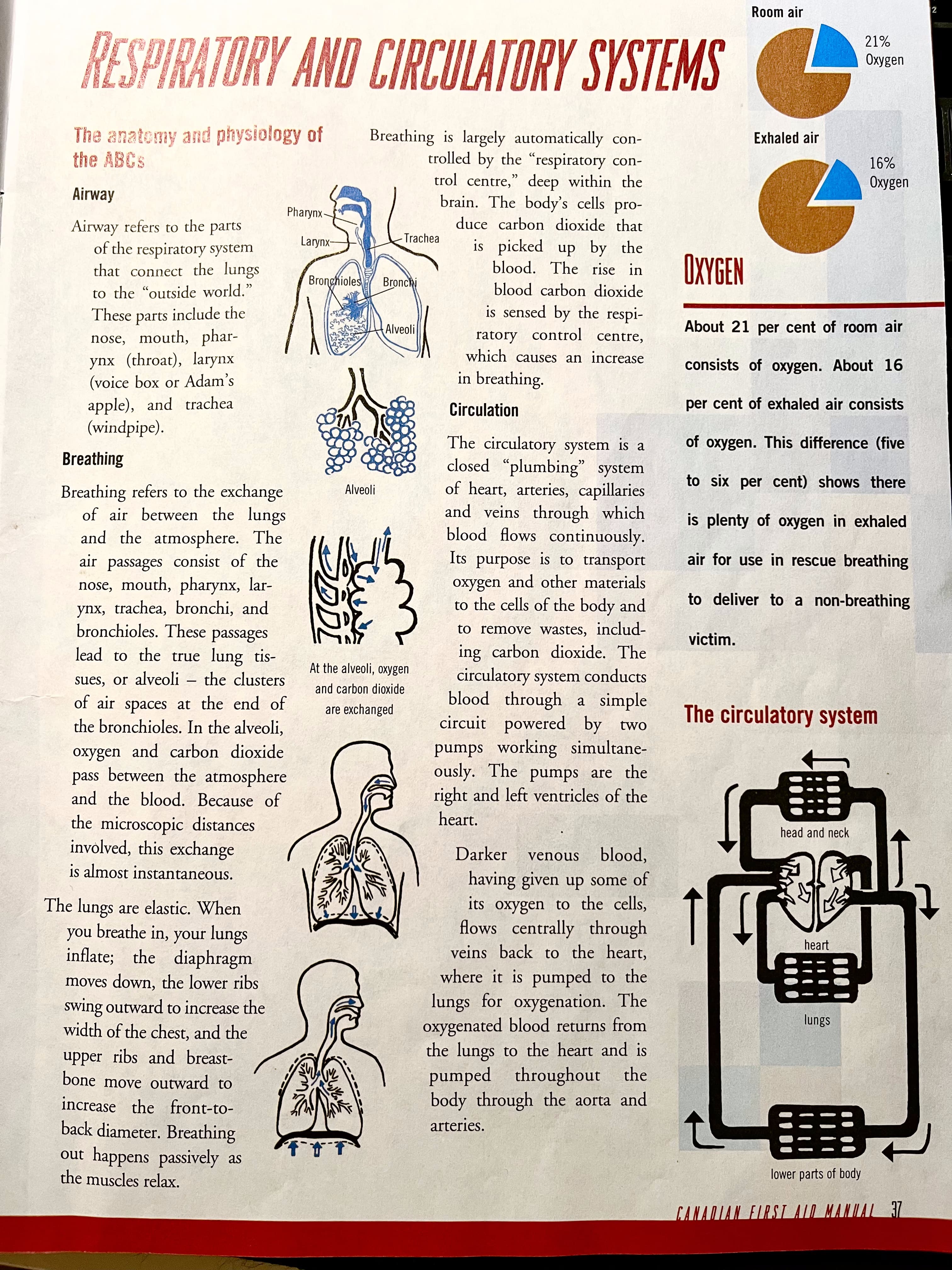
ABC
CRS
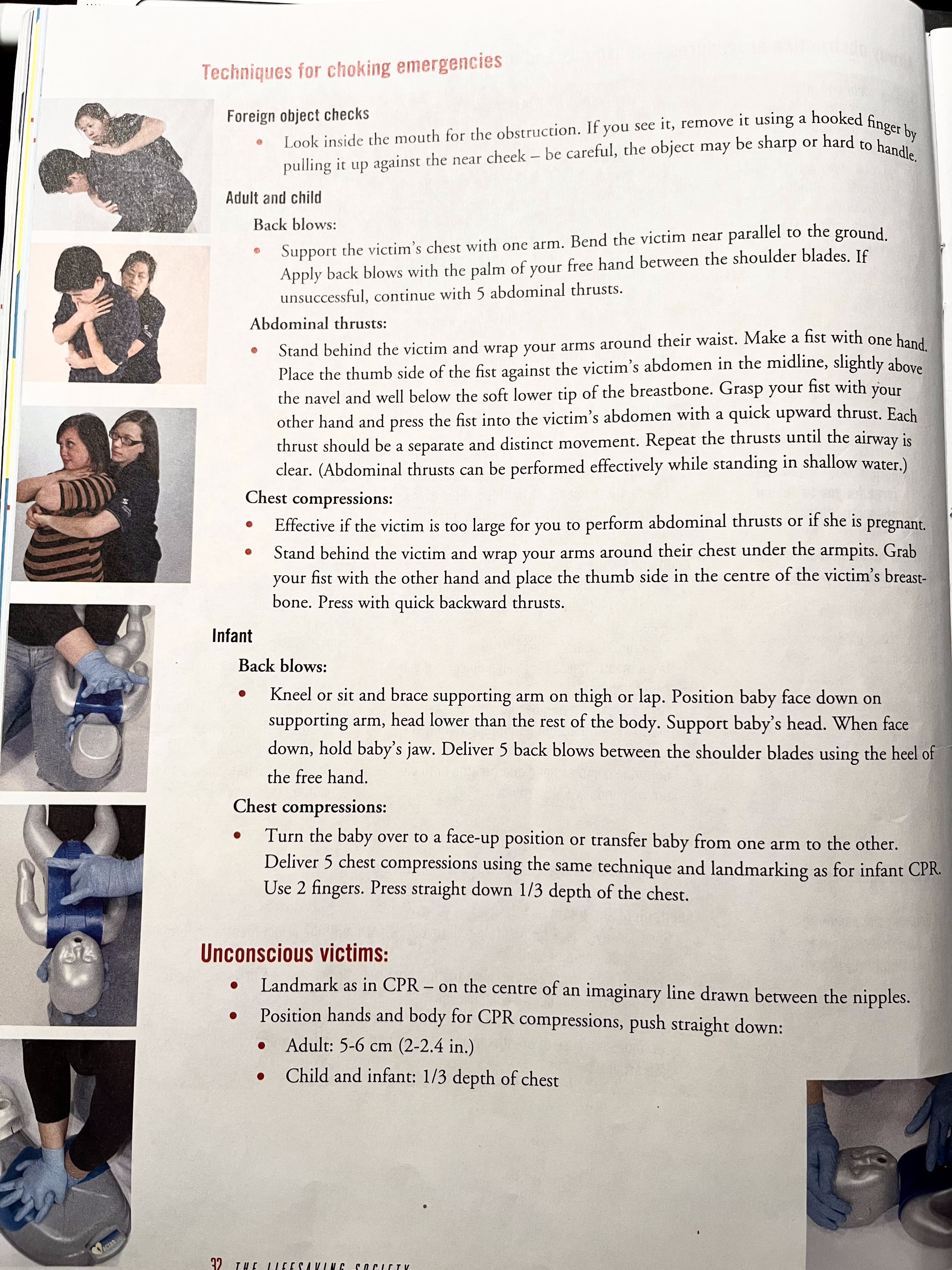
Chocking
Injuries
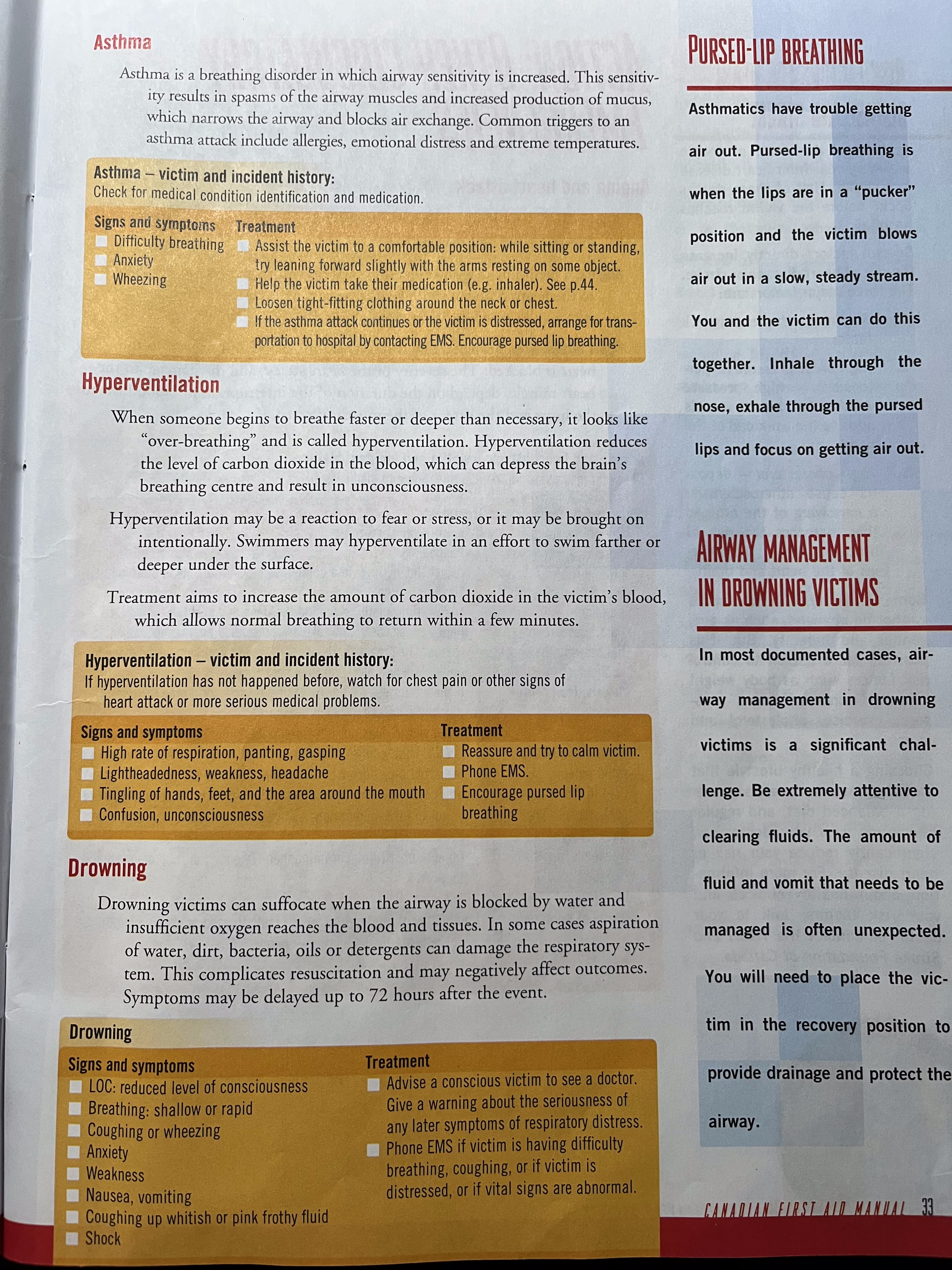
Asthma
Hyperventilation
Drowning
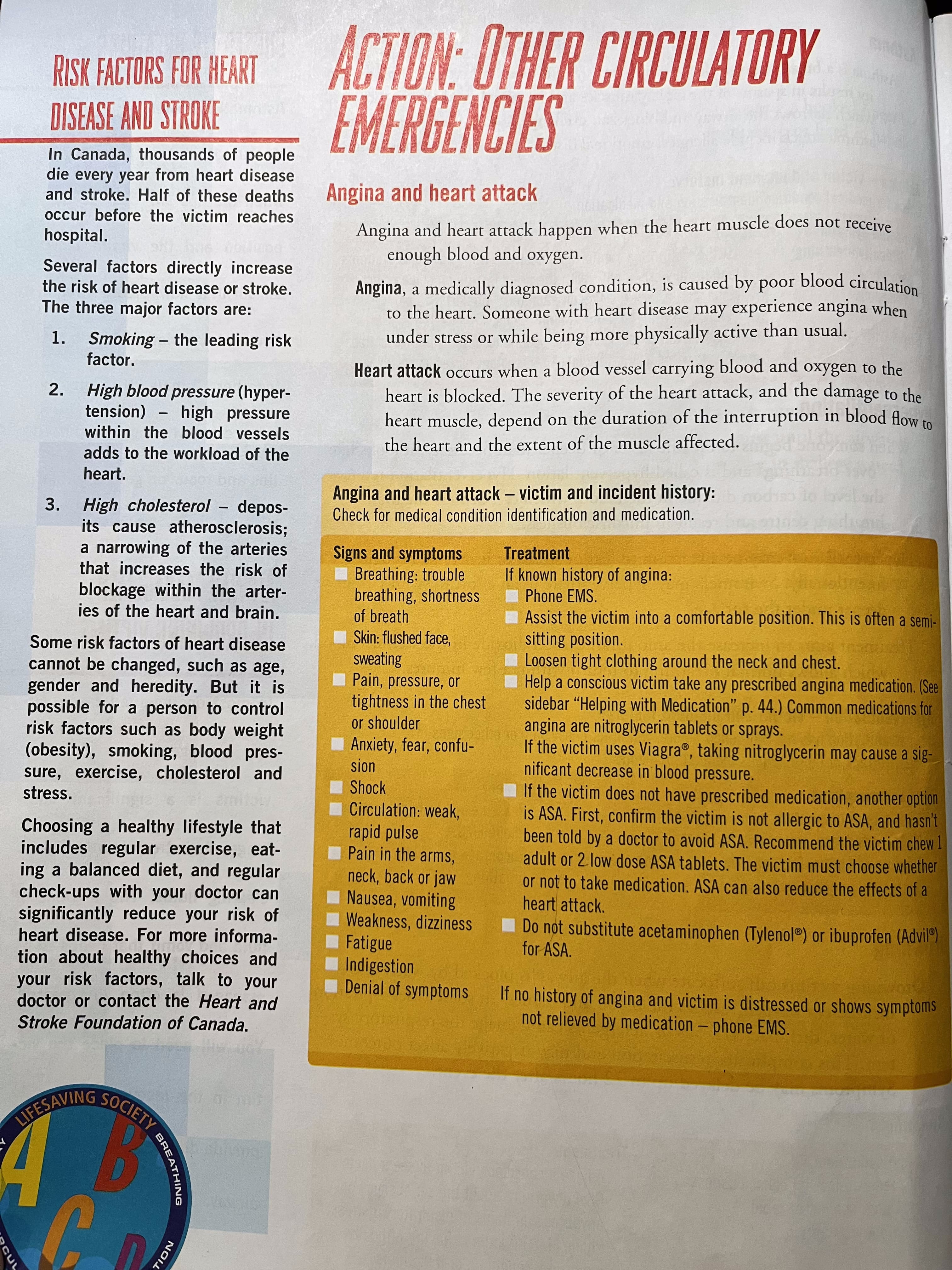
Angina and heart attack
Stroke
Shock
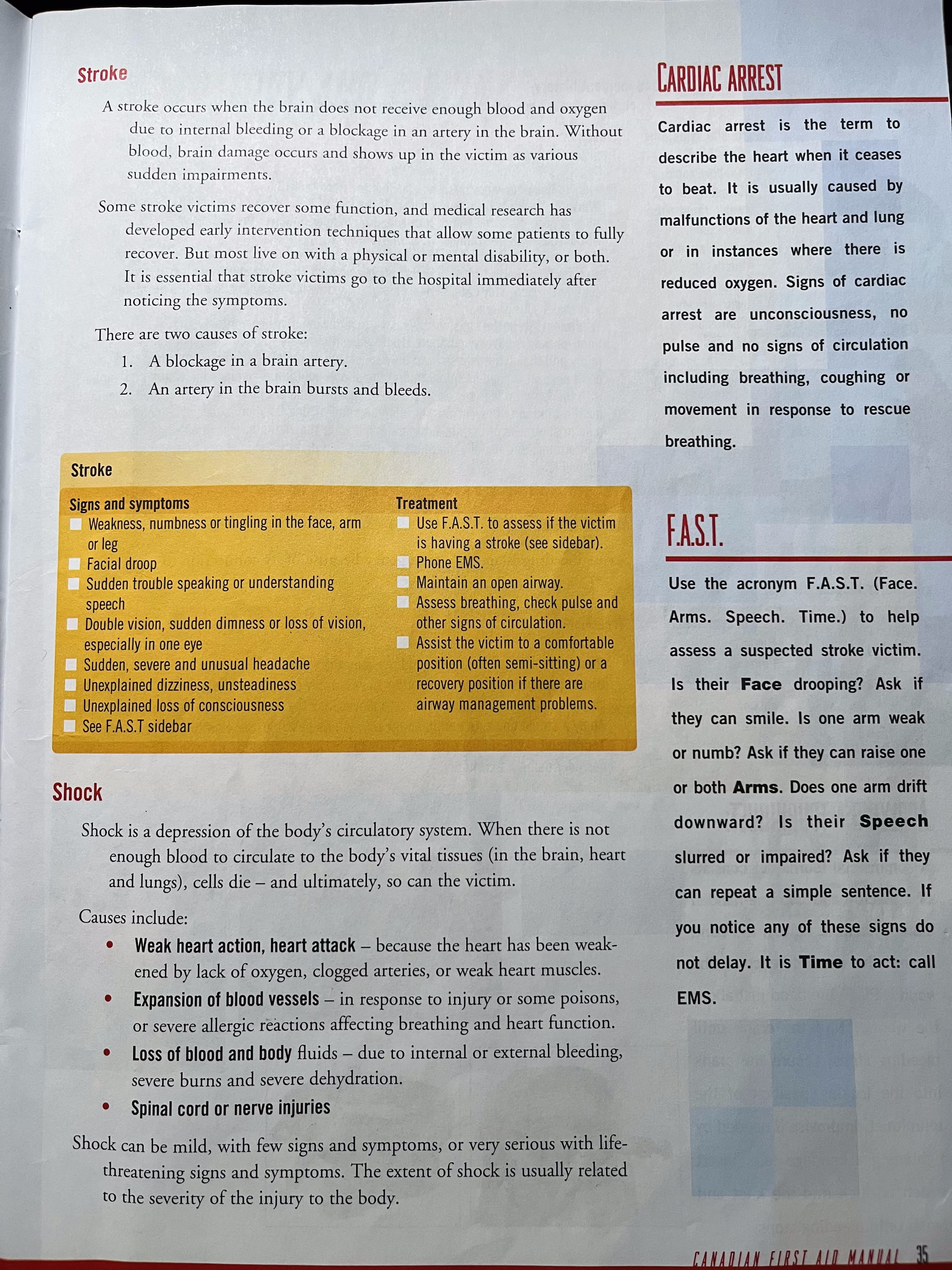
stroke:
- facial droop
- arms - can they raise one or both arm, can they strength both hands
- speech
- time - how long since the symptoms happens
shock:
w - warmth
a - ABCs
r - rest and reassurance
t - treatment -> the cause of the shock
s - semi-prone (recovery) position
Bleeding
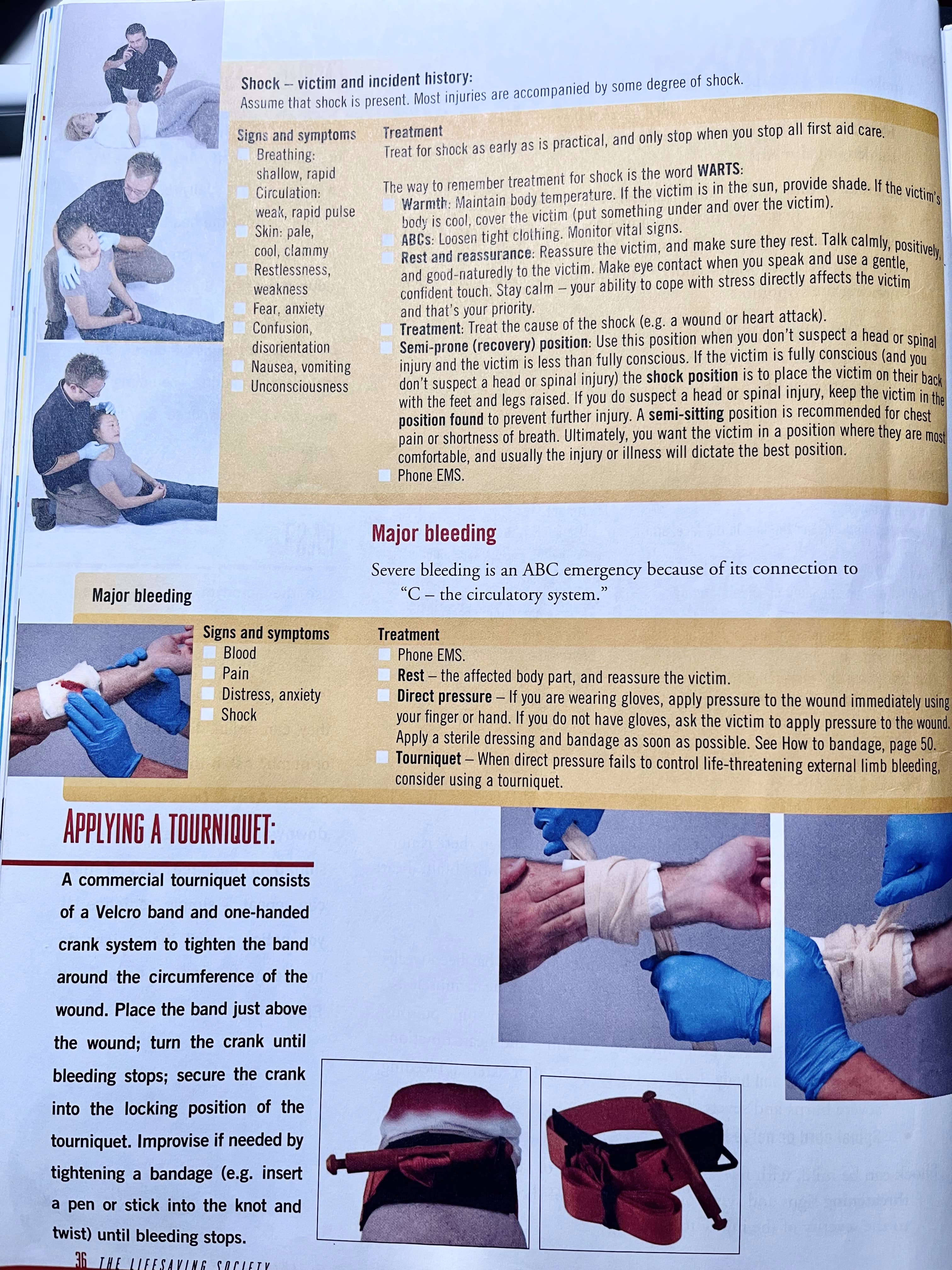
major bleeding:
- direct pressure, pinch the area
- rest reassure
- shock
Arterial
With this type of bleeding, the blood is typically bright red to yellowish in colour, due to the high degree of oxygenation. A wound to a major artery could result in blood ‘spurting’ in time with the heartbeat, several meters and the blood volume will rapidly reduce.
Venous
This blood is flowing from a damaged vein. As a result, it is blackish in colour (due to the lack of oxygen it transports) and flows in a steady manner. Caution is still indicated: while the blood loss may not be arterial, it can still be quite substantial, and can occur with surprising speed without intervention.
Capillary
Bleeding from capillaries occurs in all wounds. Although the flow may appear fast at first, blood loss is usually slight and is easily controlled. Bleeding from a capillary could be described as a ‘trickle’ of blood.
The key first aid treatment for all of these types of bleeding is direct pressure over the wound.
Priority of treatment
Priority of treatment
- Breathing
- Bleeding
- Brains
- Bones
Secondary Emergencies
Care for other injuries and illness.
Main steps:
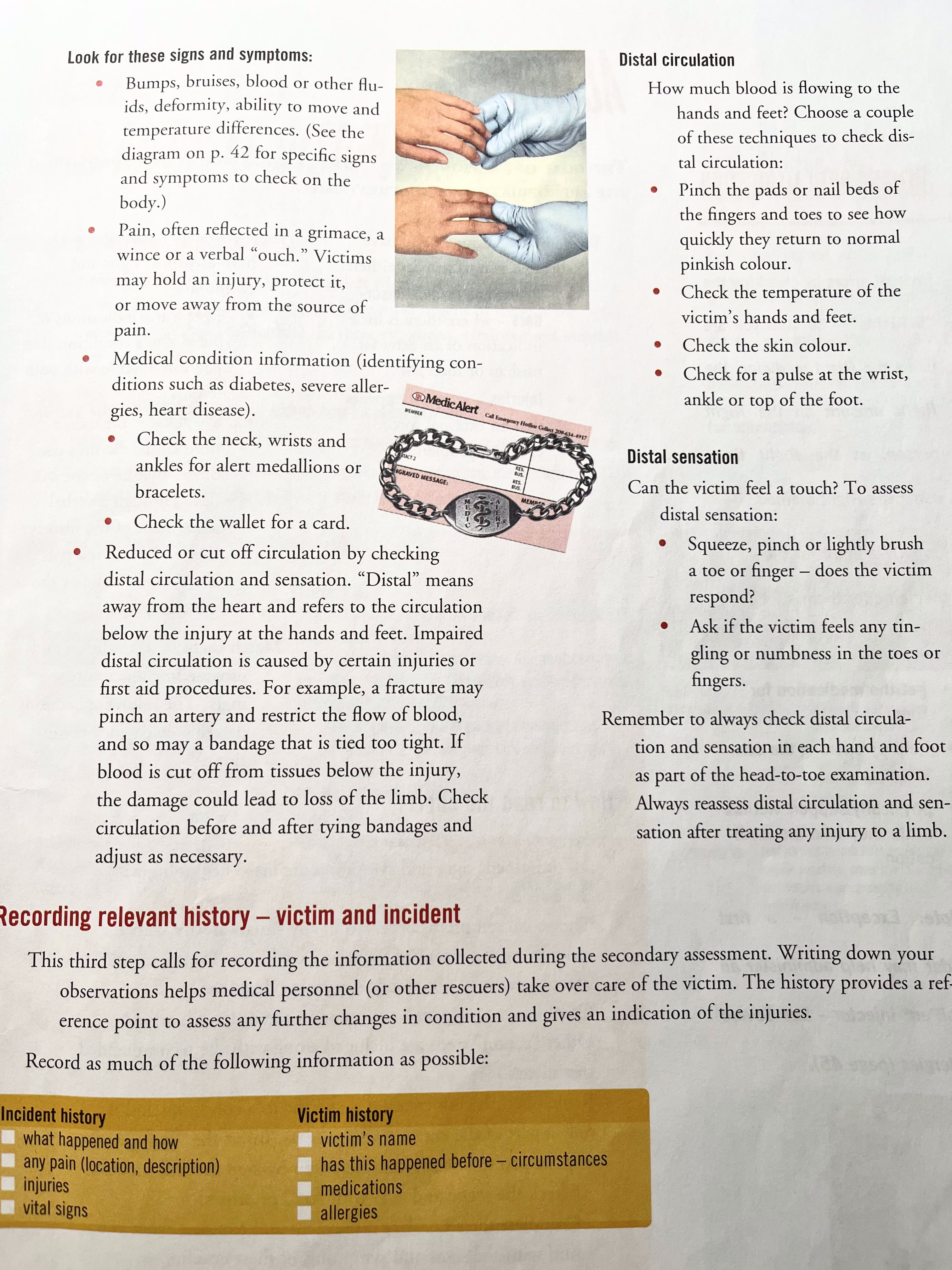
- relevant history, PCSAMPLEs
- vital signs
- head to toe examination -> find the injury
- recheck vitals every 5-10 minutes
(History first.)
- Determine what is wrong, and determine if other potential injuries, illnesses or complicating factors exist. Is the injury a result of an external force, or is this a medical disorder or illness.
- Point to the appropriate action and treatment.
- Gather information to pass on to medical or emergency personnel.
PCSAMPLEs
P - person: name, age, gender, pregnancy
C - chief complaint
S - signs/symptoms
A - allergies
M - medications
P - post medical conditions
L - last oral intake
E - events prior
Vital signs:
- LOC(level of consciousness) - AVPU (ongoing assessing)
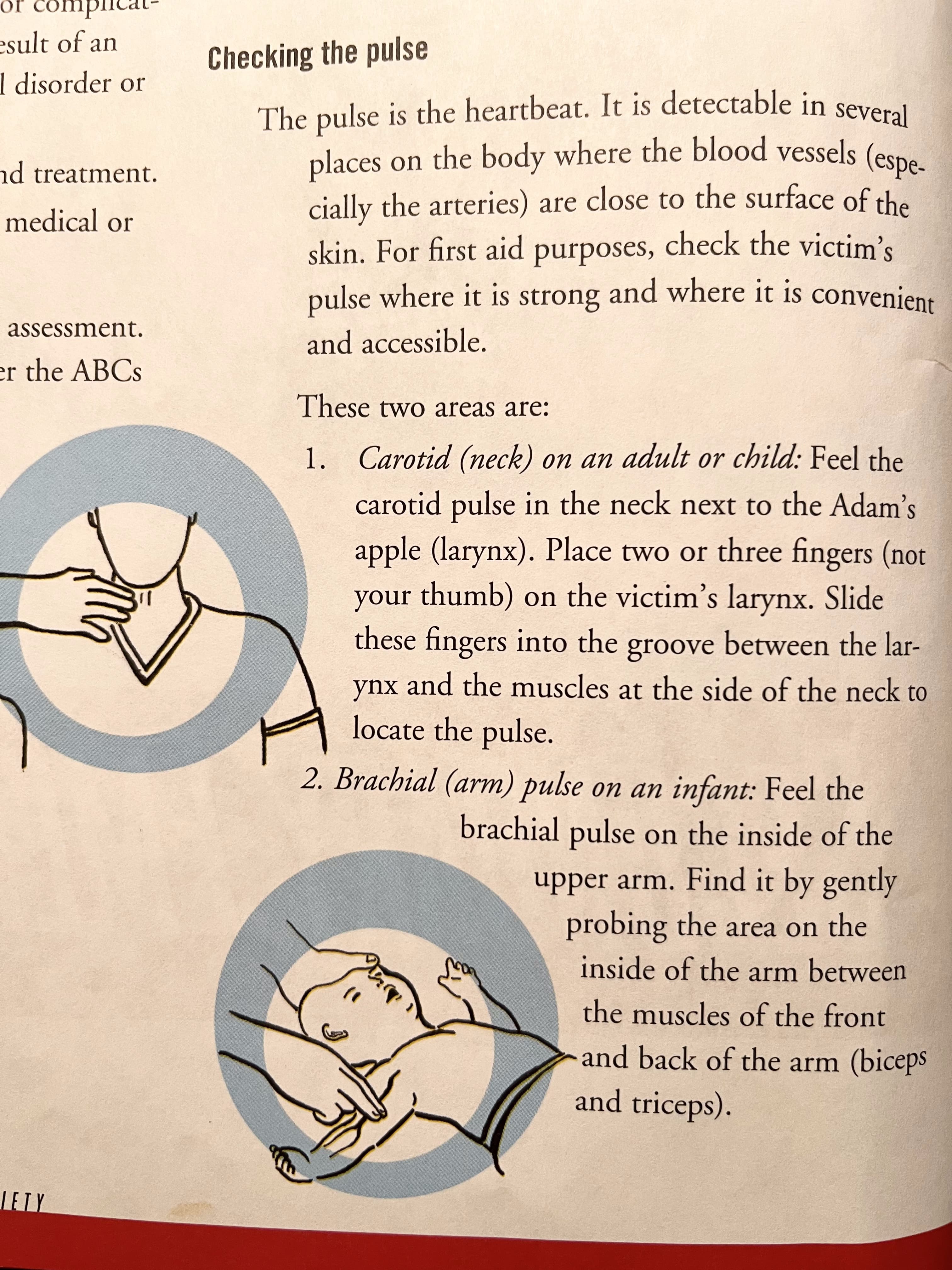
- Pulse - rate/ rhythm/ depth (15 sec -> times 4, or 10s, but 15 may be better, 60~100/120 bpm, regular or irregular, sallow/ normal/ deep)
- Breathing - rate/ rhythm/ depth (12-24bpm)
- Skin - colour(finger nails, lips inside), texture (moisture, sweety), temperature
- Pupils -> (or ask them to close, then open) bright light, close pupils, flashlight from right to left, # -> 3-4mm, pupil equal and reactant light
Checking the pulse
Head to toe examination
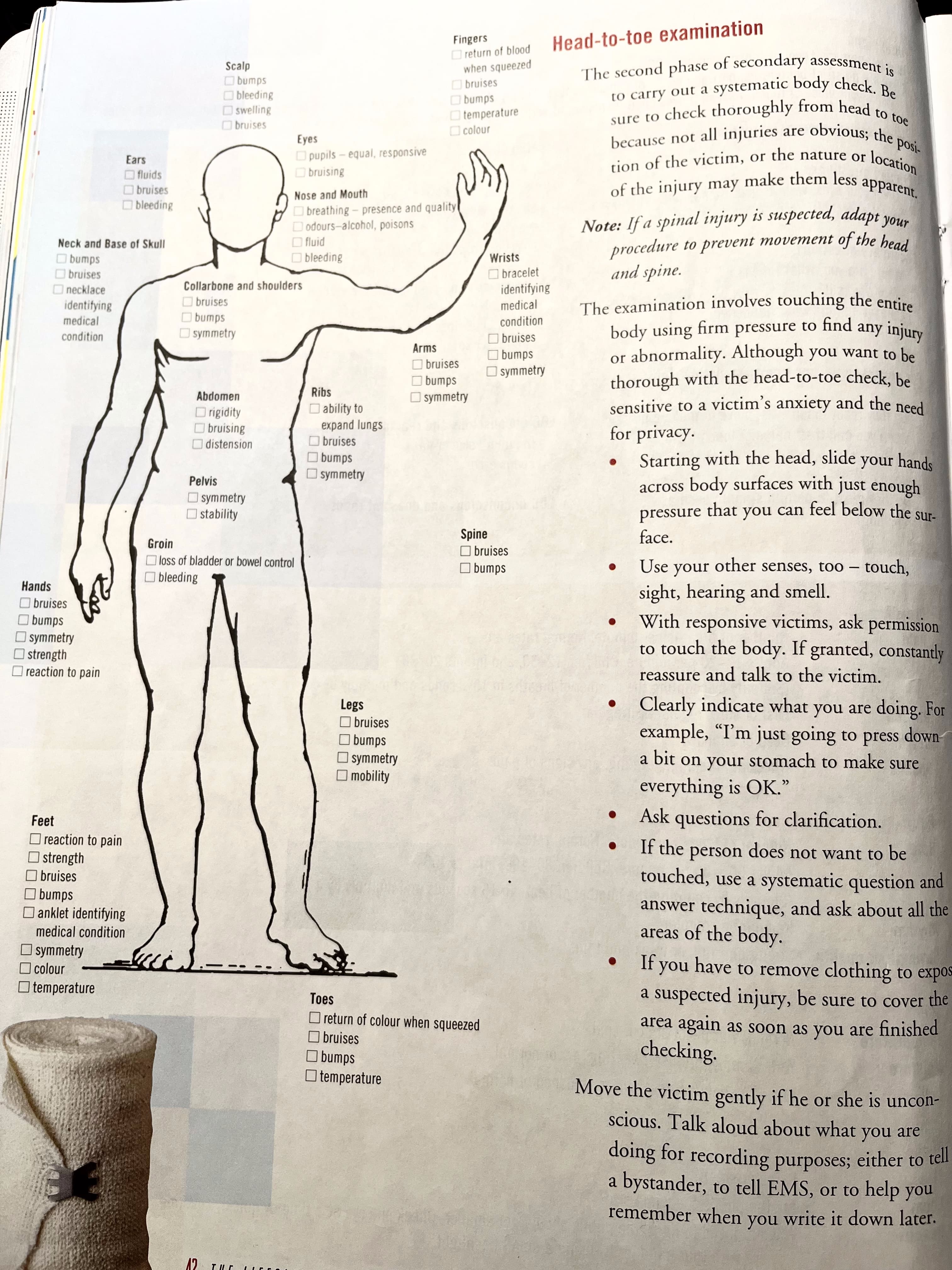
Exam from top of the head, ask do victim feel anything, any pain or sensitivity.
When checking, check bleeding, check joints, fluid (white/ yellow-ish spanish fluid), looking for breaking bones
Can victim to do head to toe themselves.
Medication rights
medication: 5 rights
- right medicine
- right person
- right amount
- right time
- right method
Illness
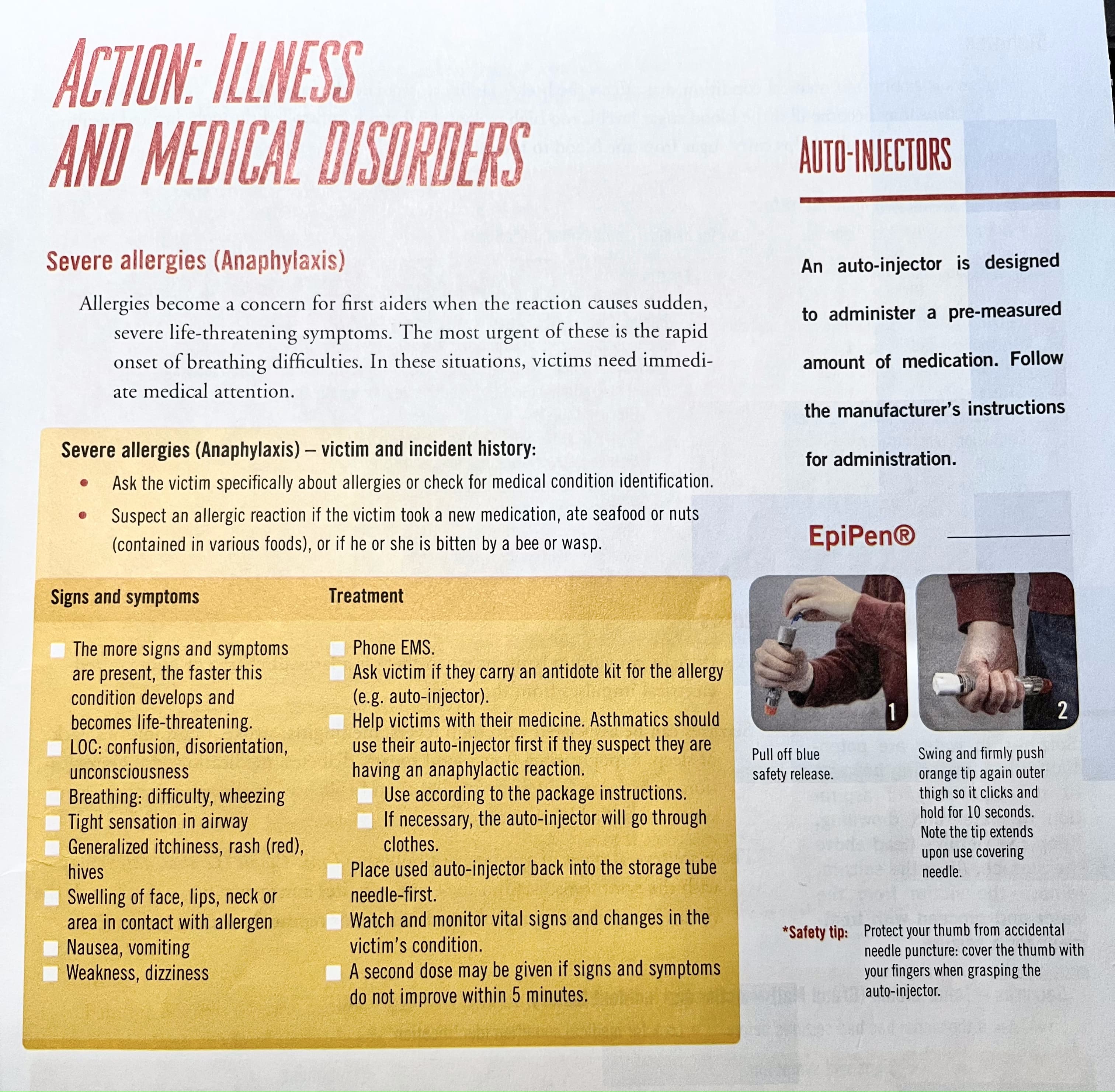
Anaphylaxis
Diabetes
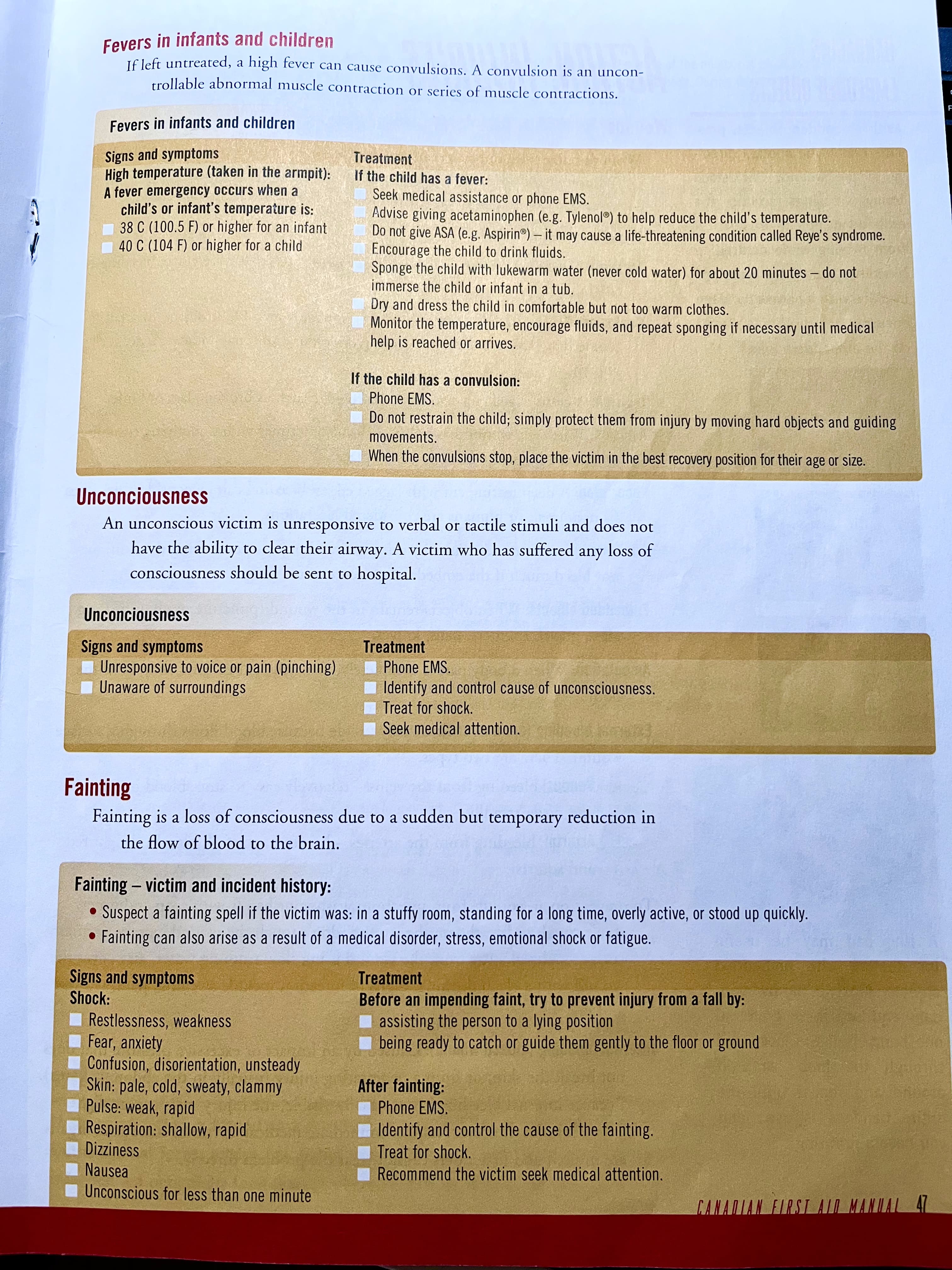
Seizures
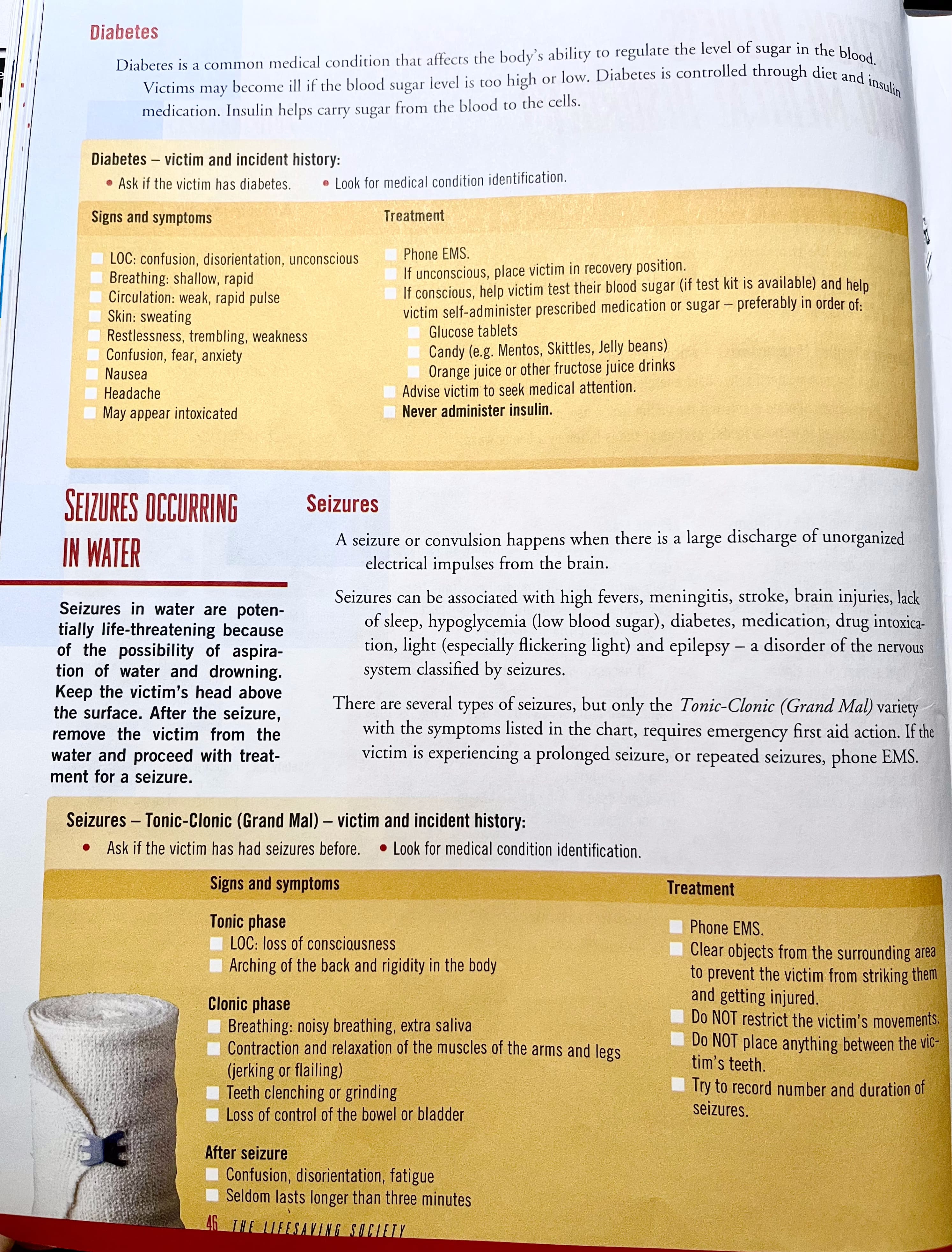
diabetes -> give sugar if diabetes shock, if then get better then better, if not 911 is on the way.
seizures -> find a nice & quite space, note down the time and duration for seizures.
Unconciousness
Fainting
Injuries
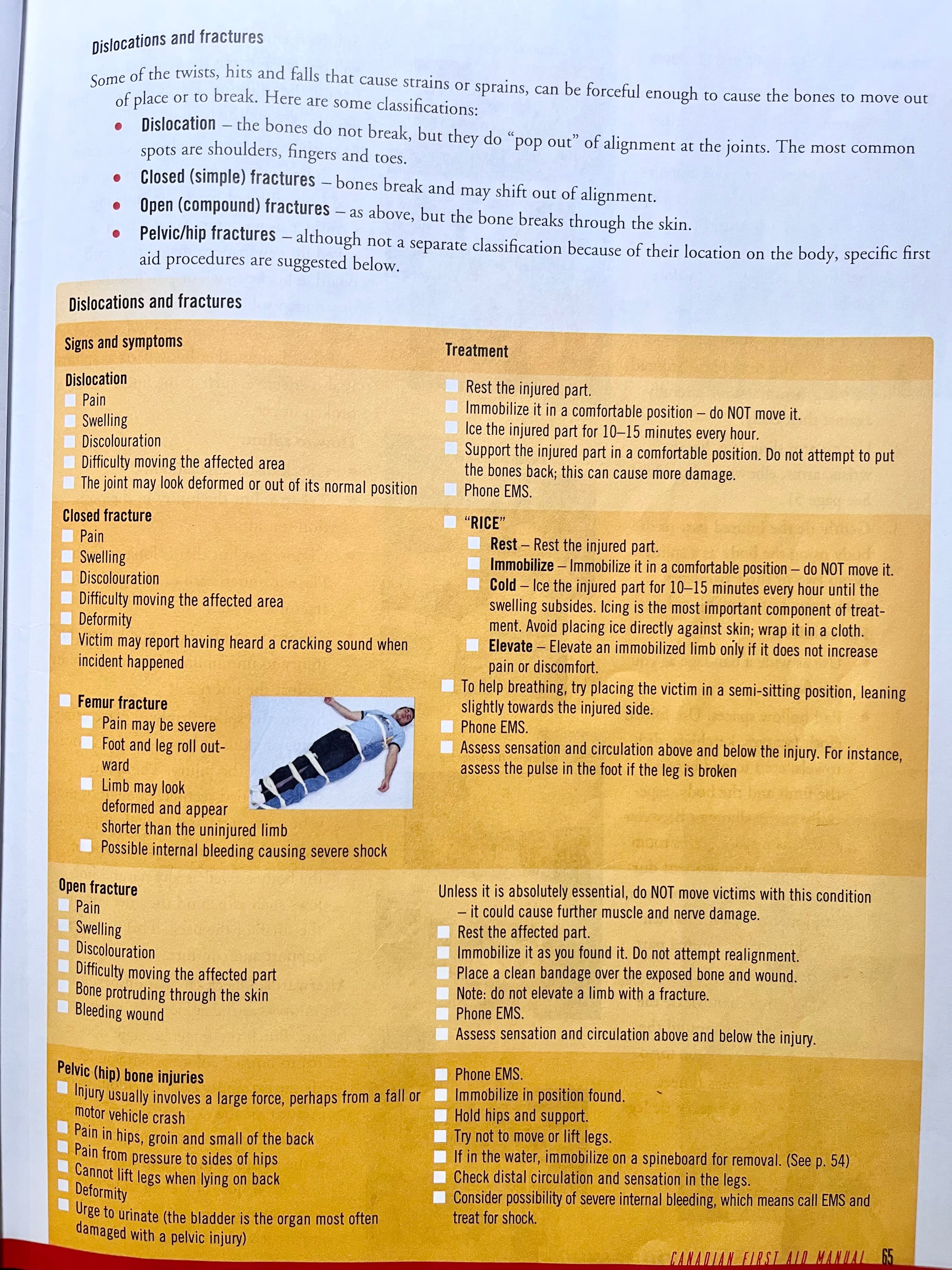
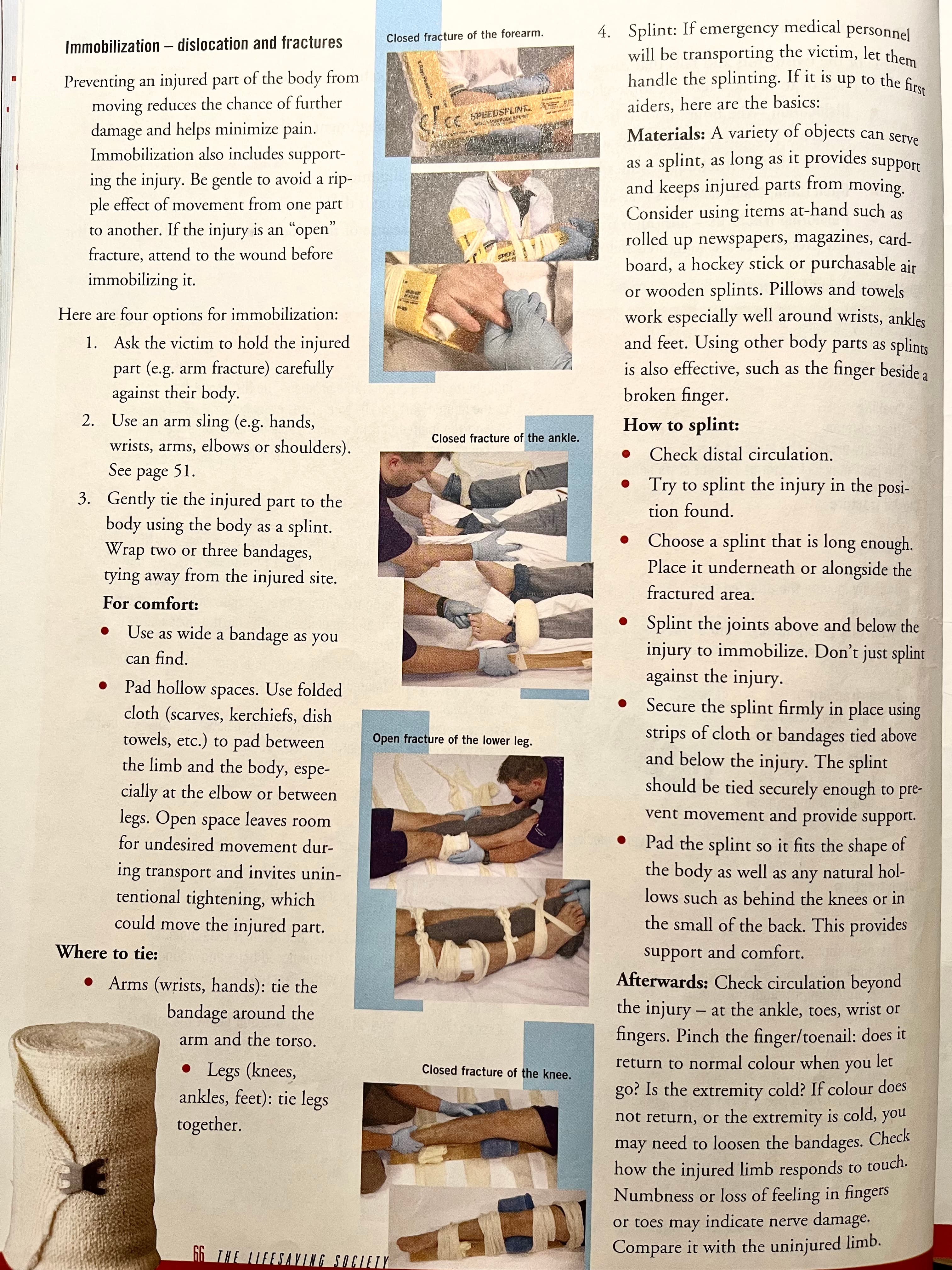
bone, joint injuries:
- R - rest reassure
- I - immobilize
- C - cold ice
- E - elevate when necessary
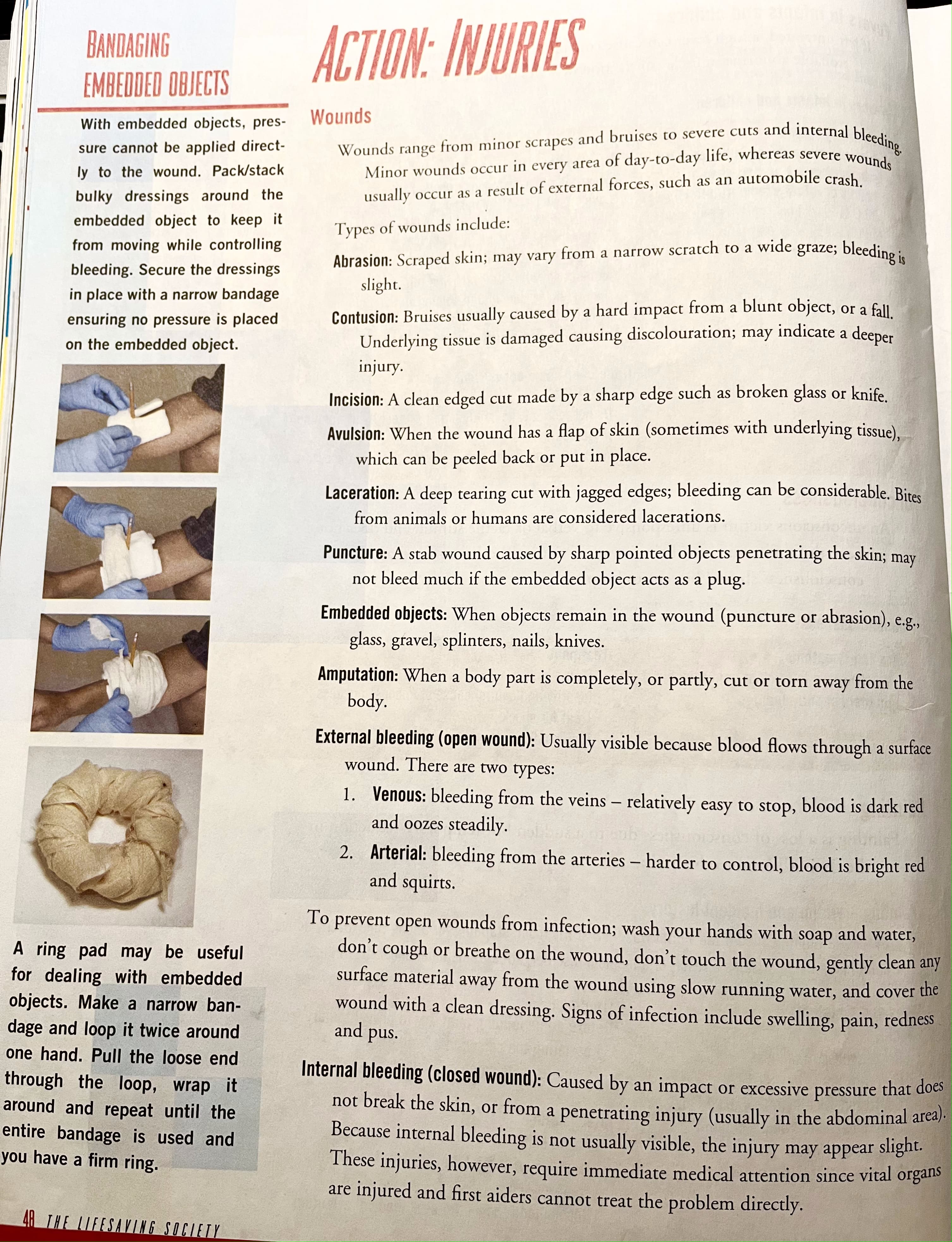
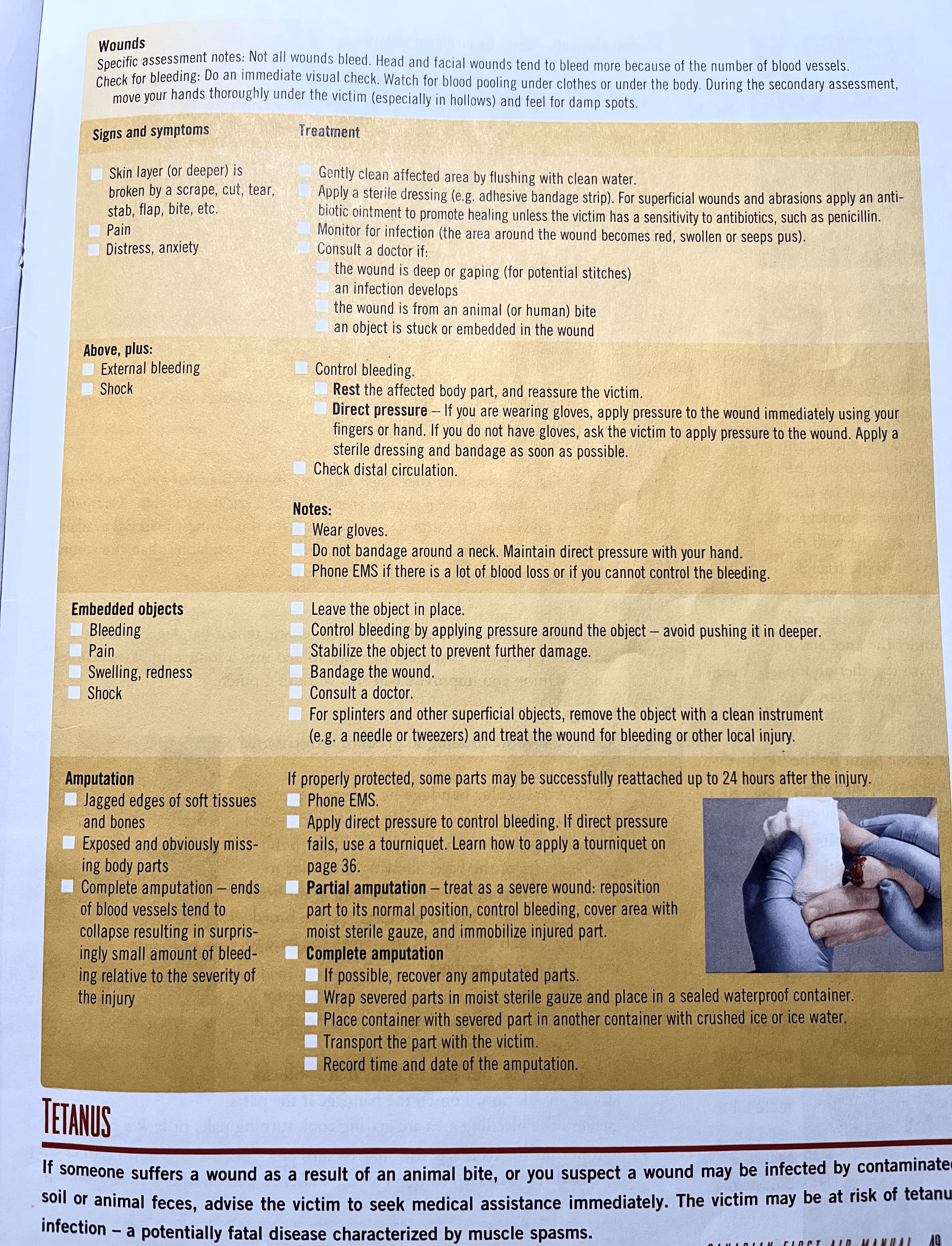
Wounds
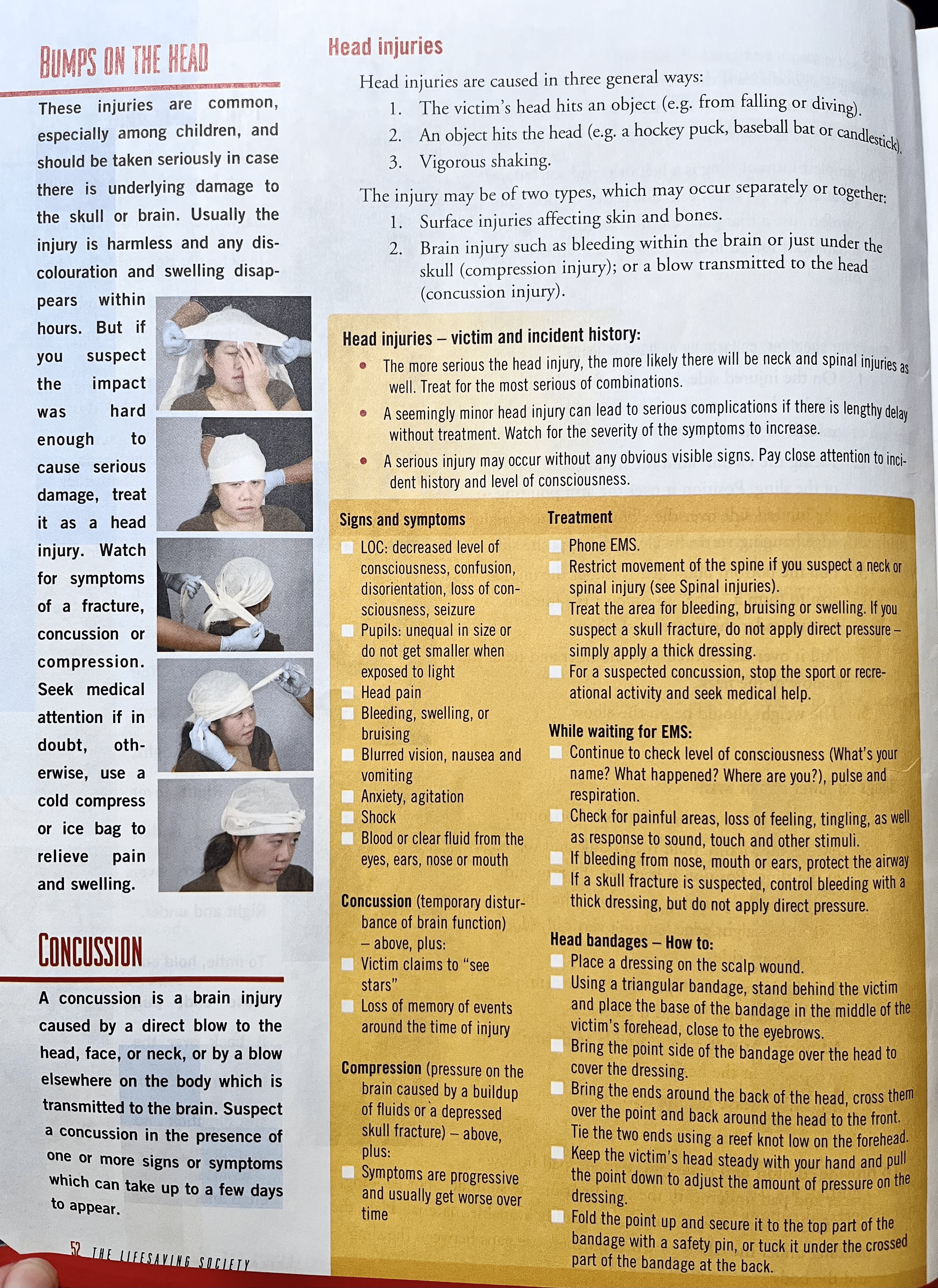
Head injuries
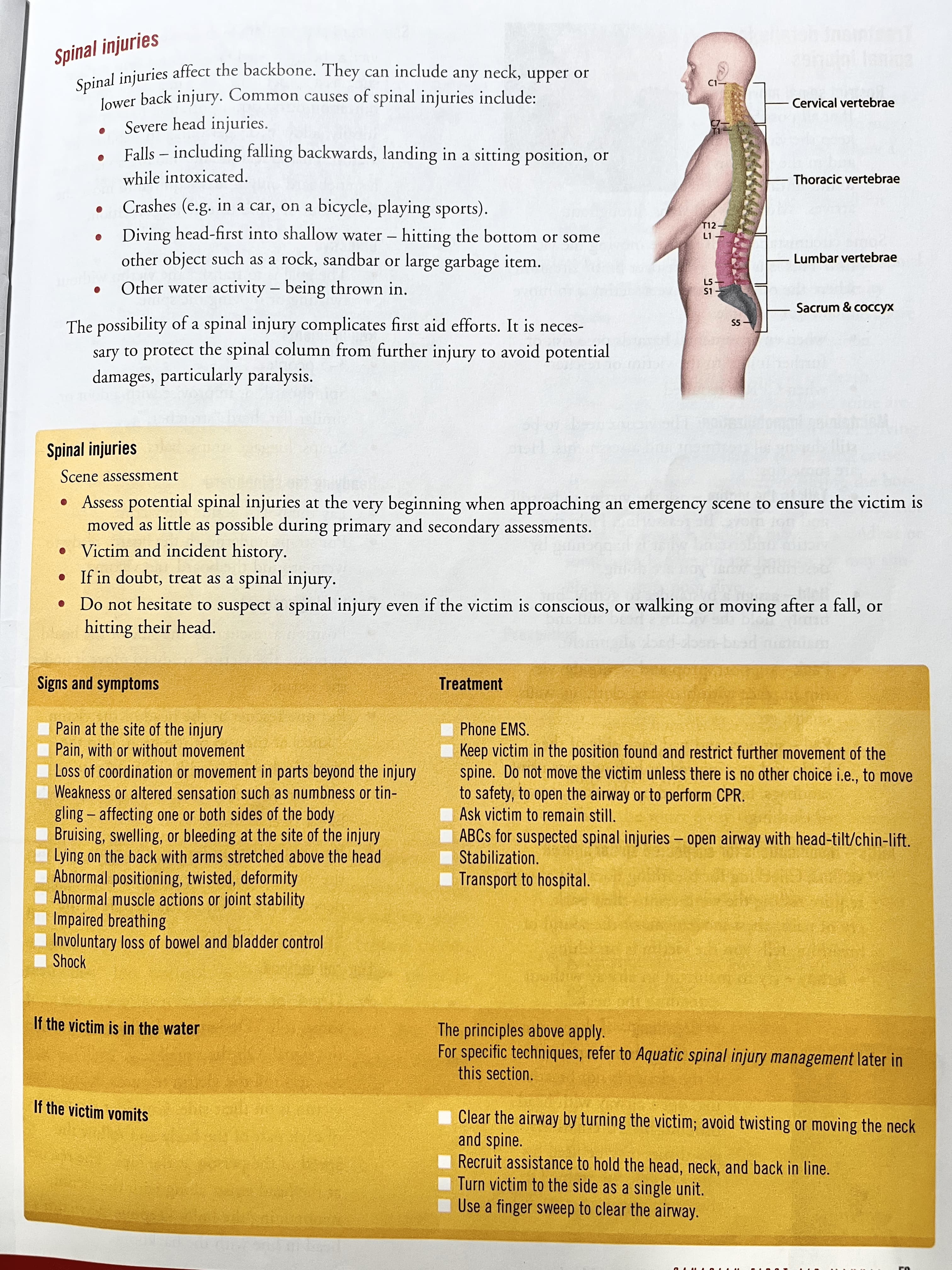
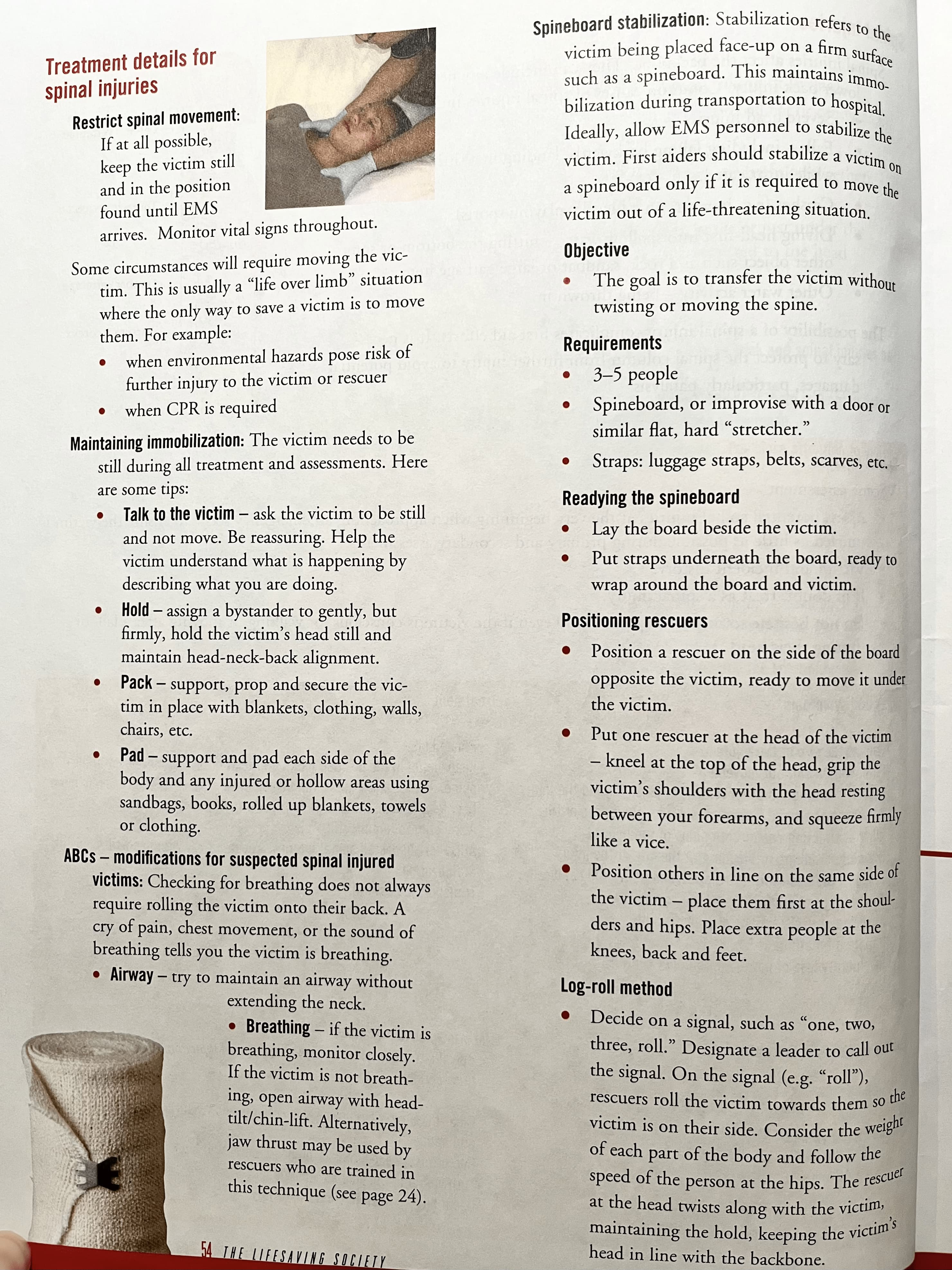
Spinal injuries
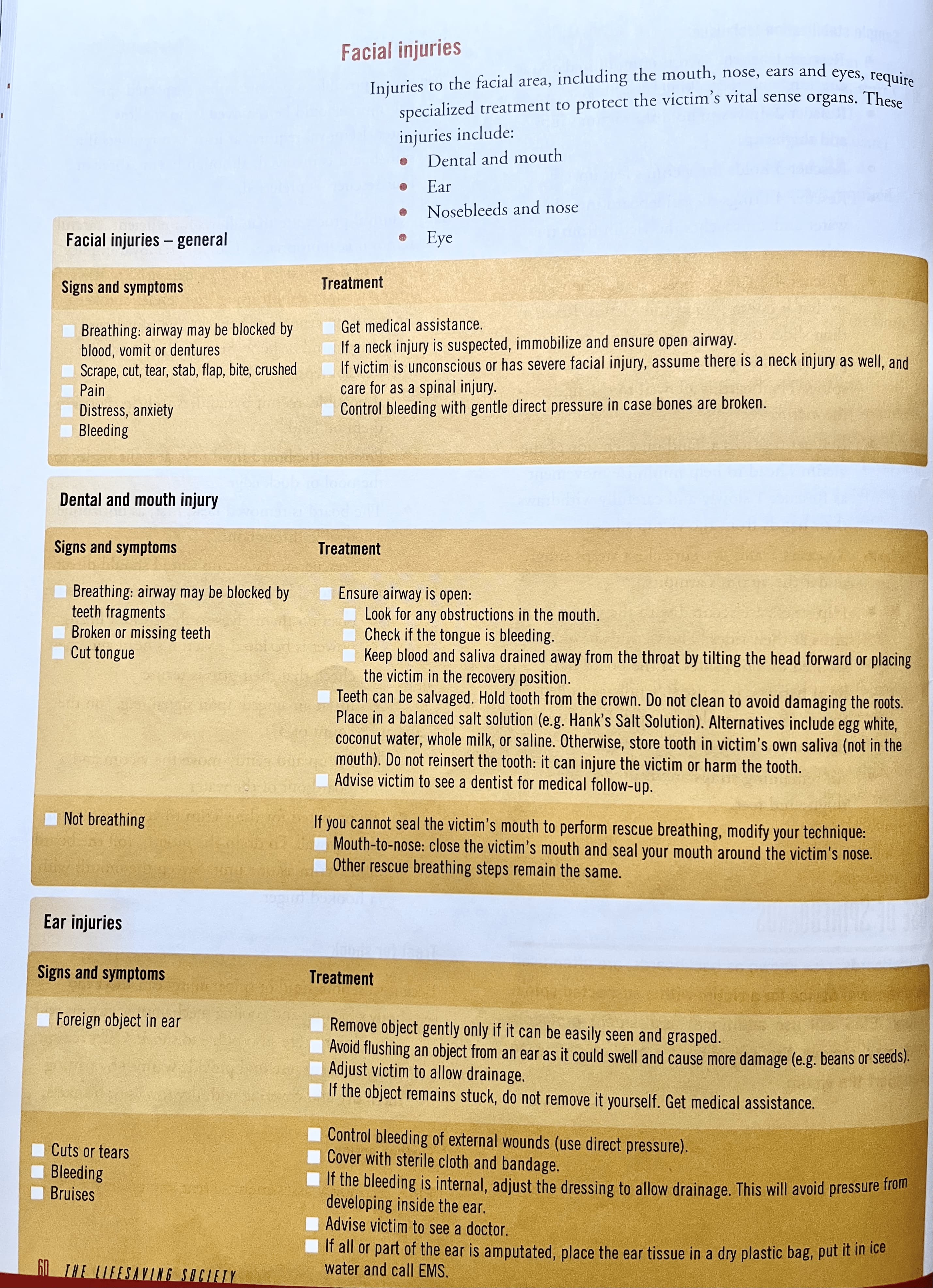
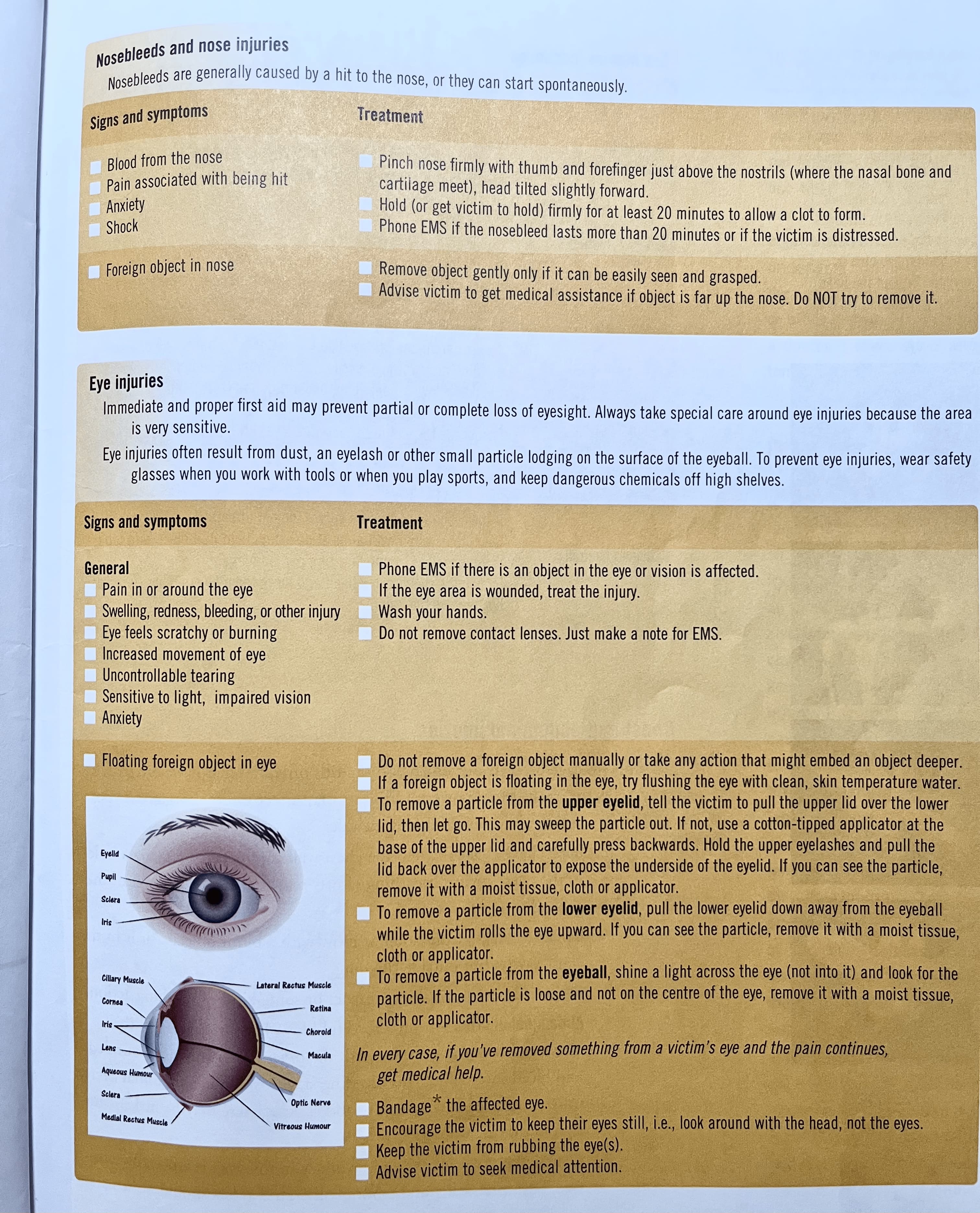
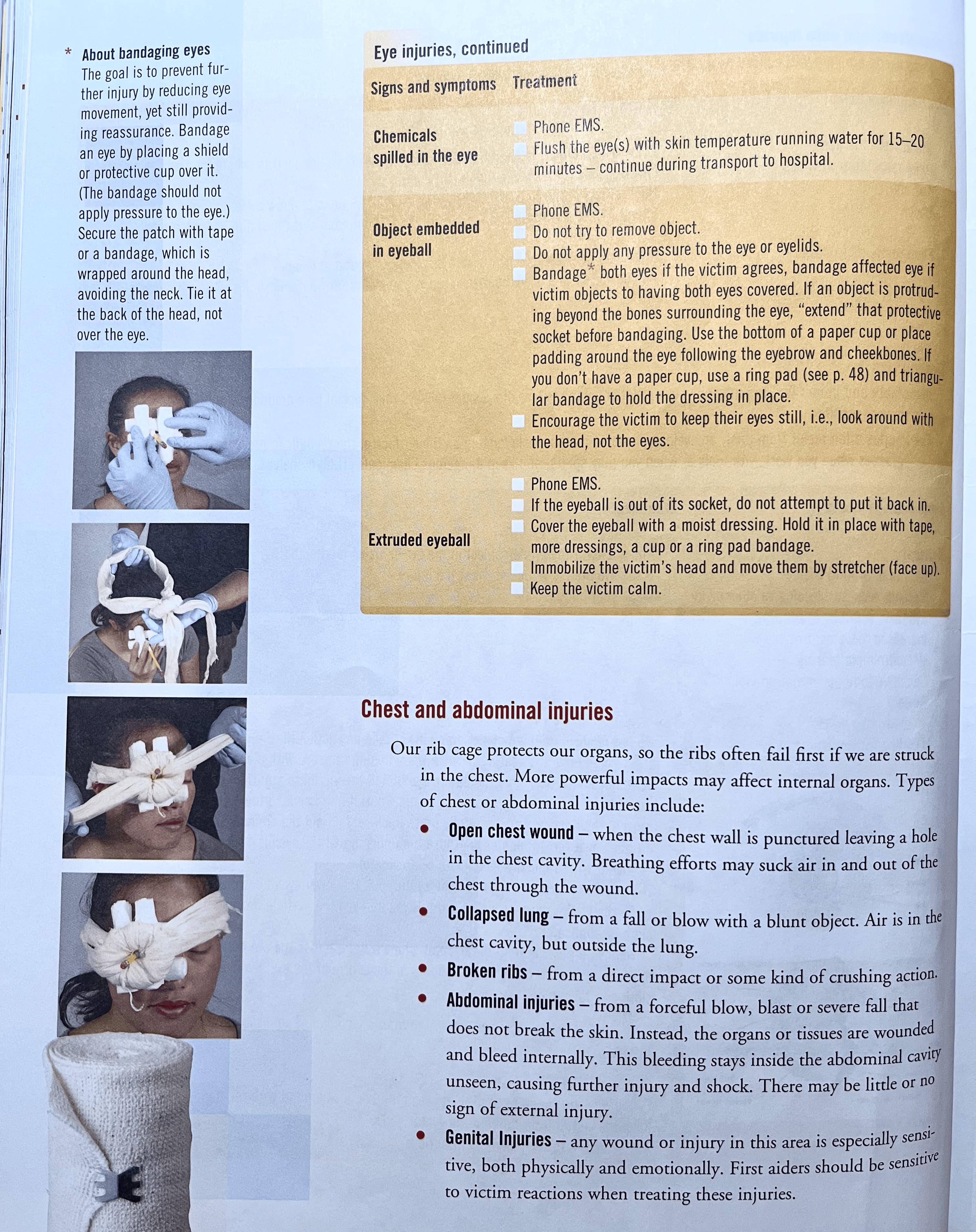
Facial injuries
Chest and abdominal rights
Bone and joint injuries
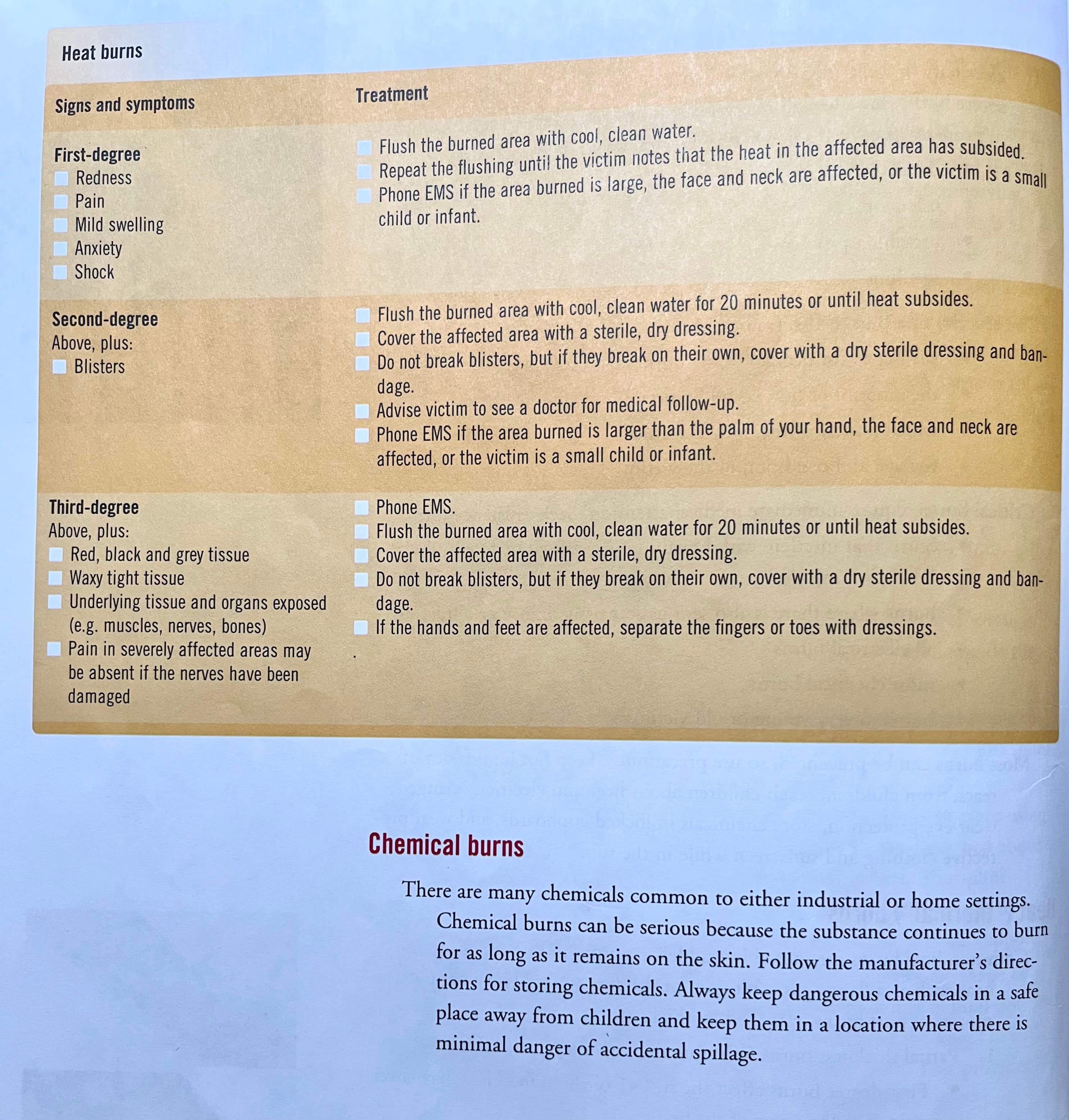
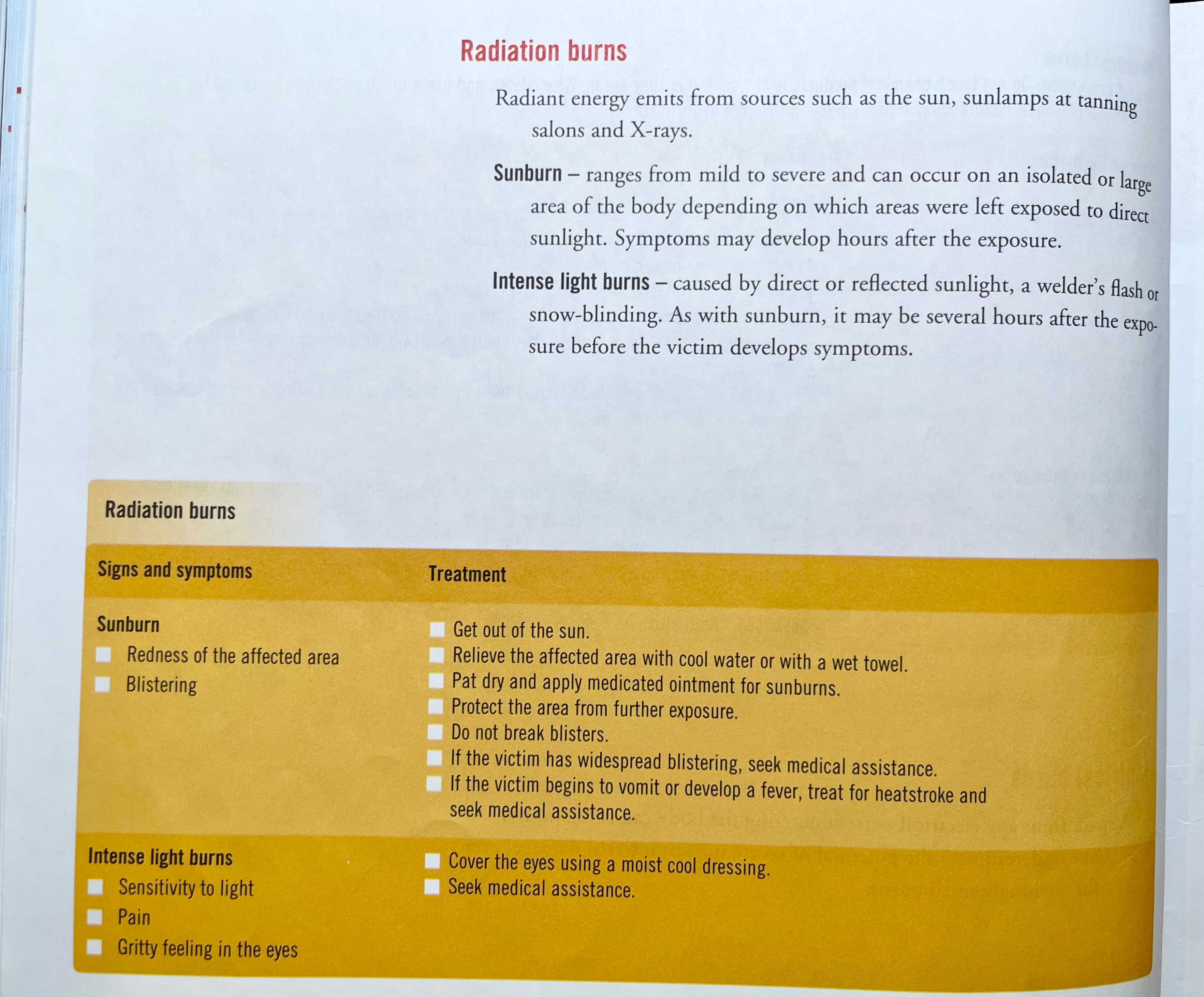
Burns
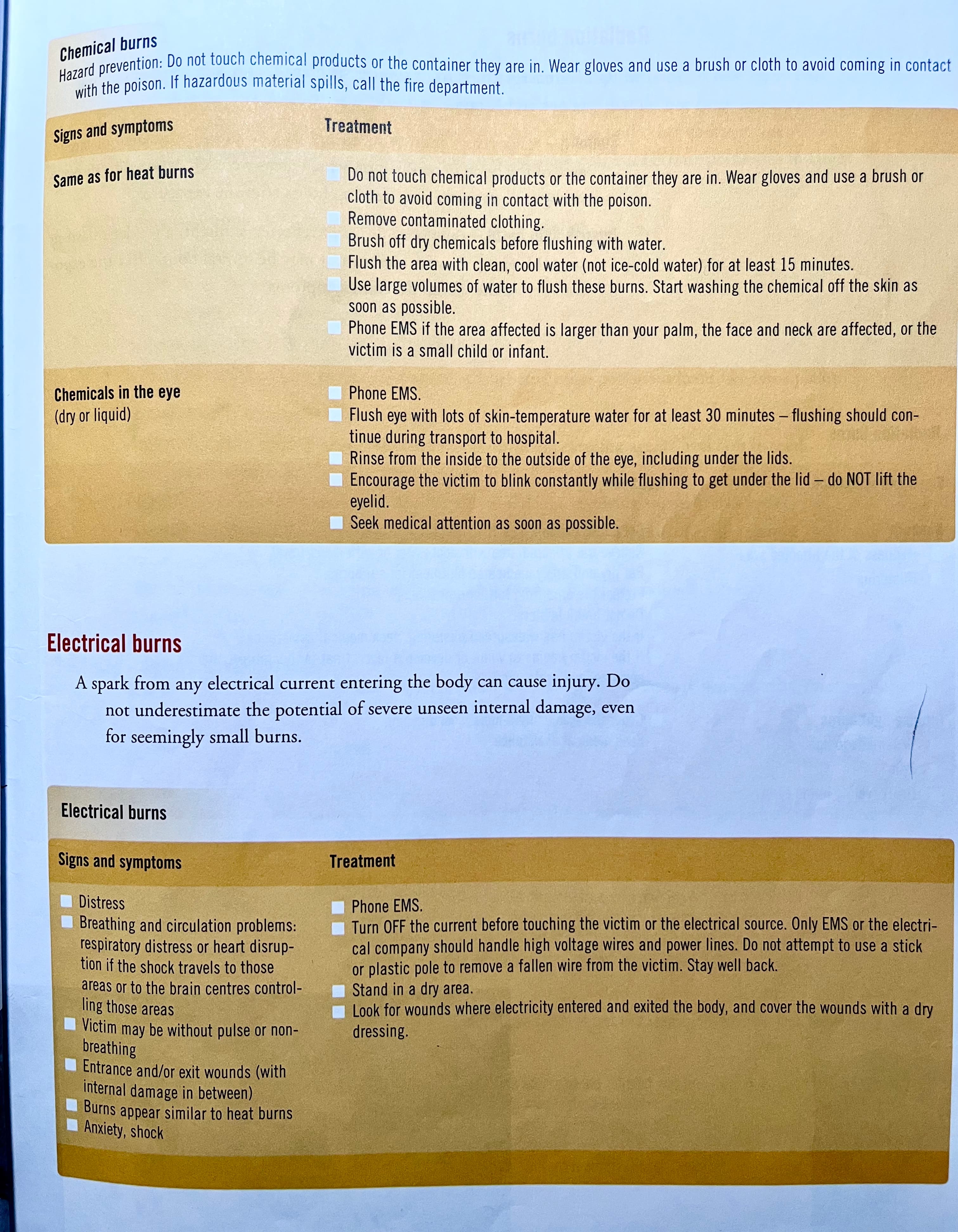
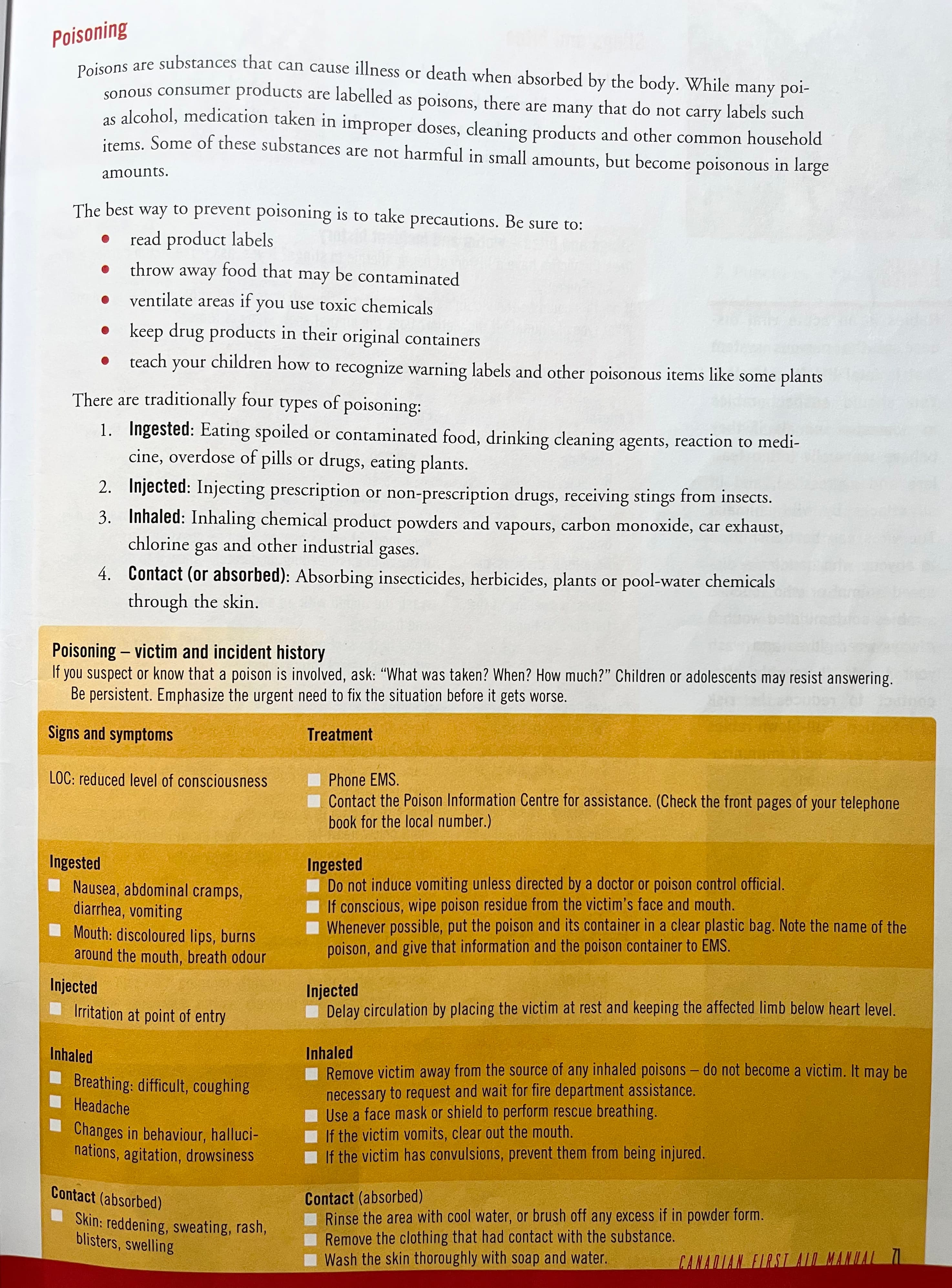
Poisoning
Stings and bites
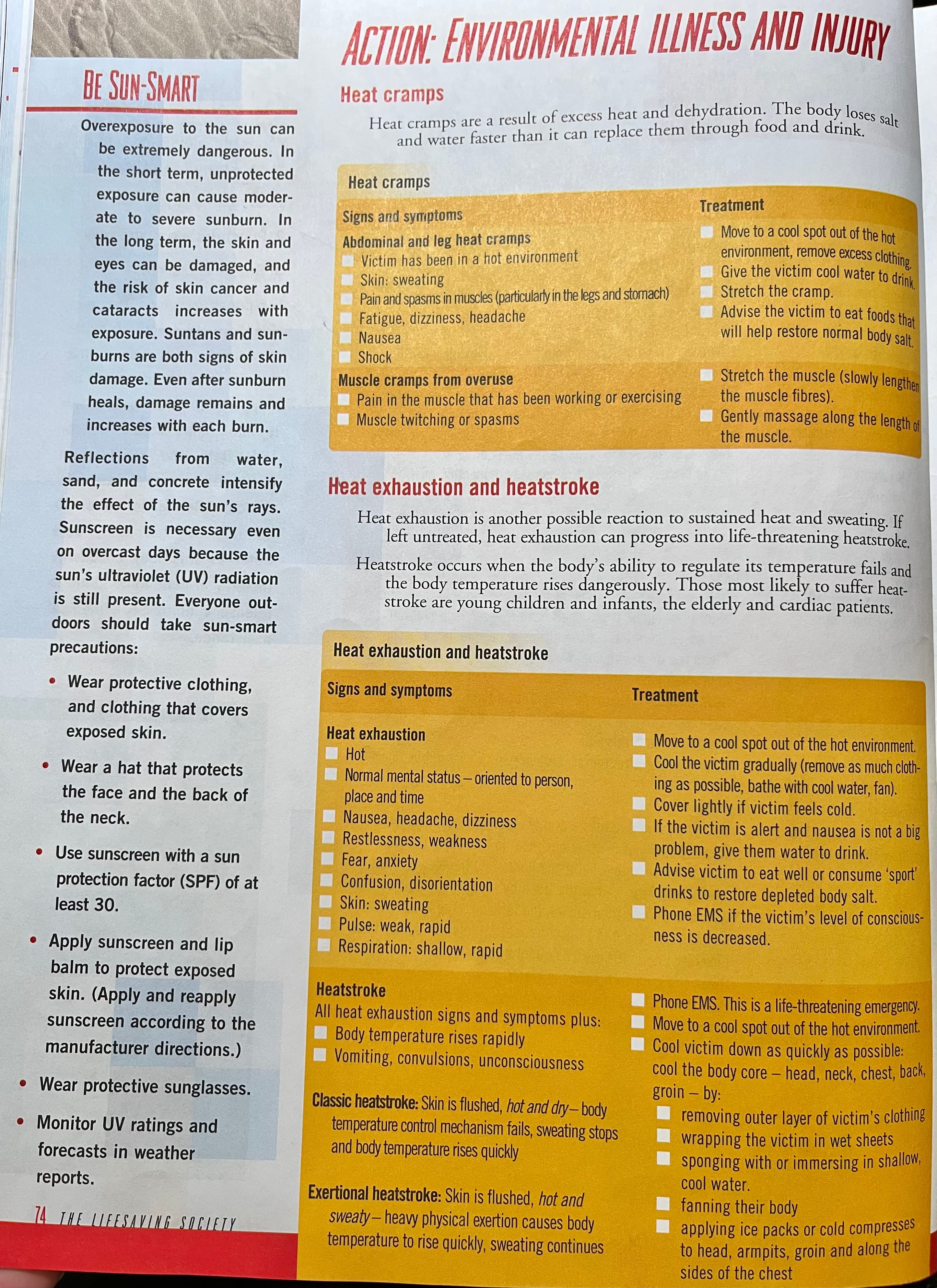
Environmental illness and injury
Heat cramps
Heat exhaustion and heatstroke
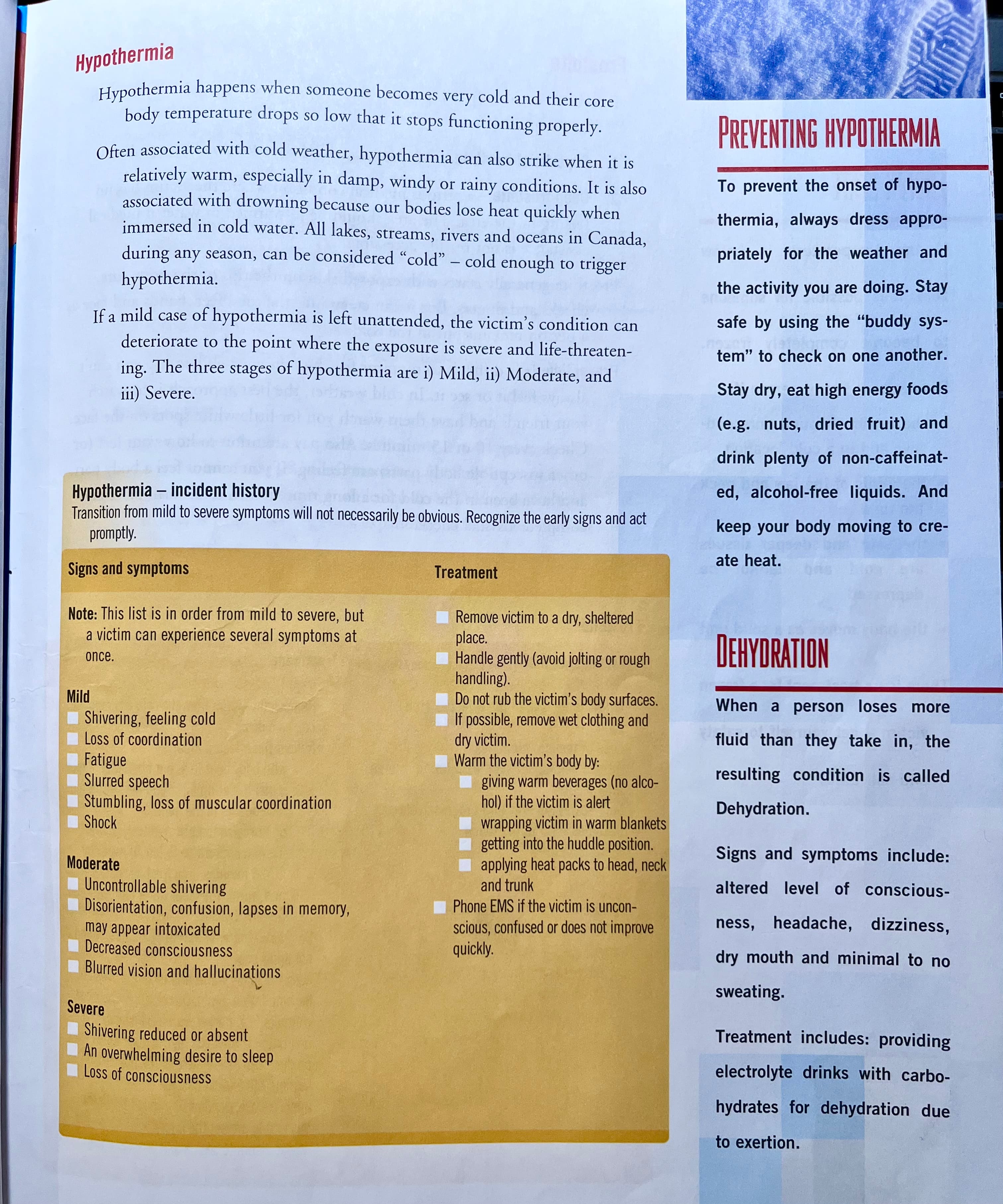
Hyothermia
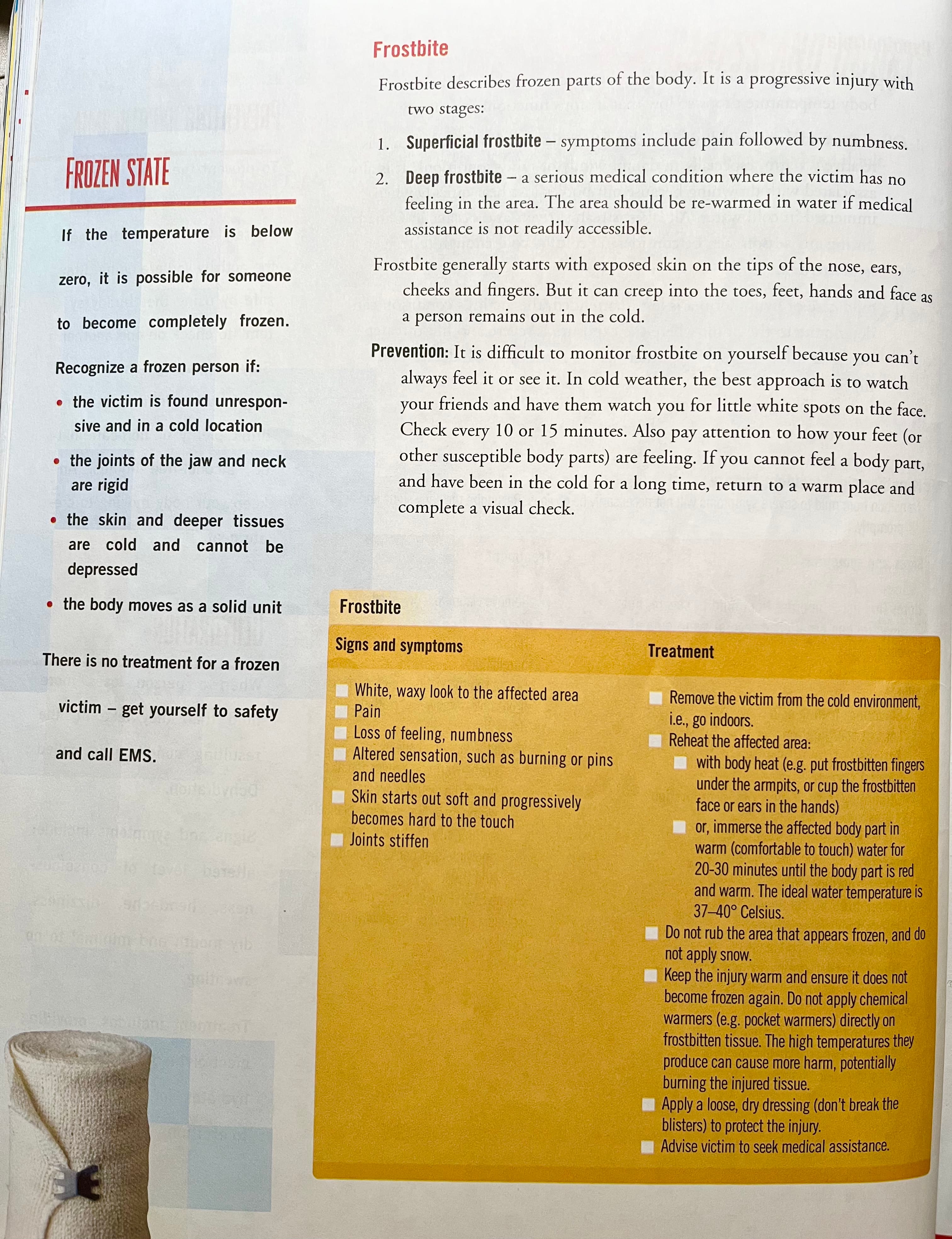
Frosbite
Pressure-related water in
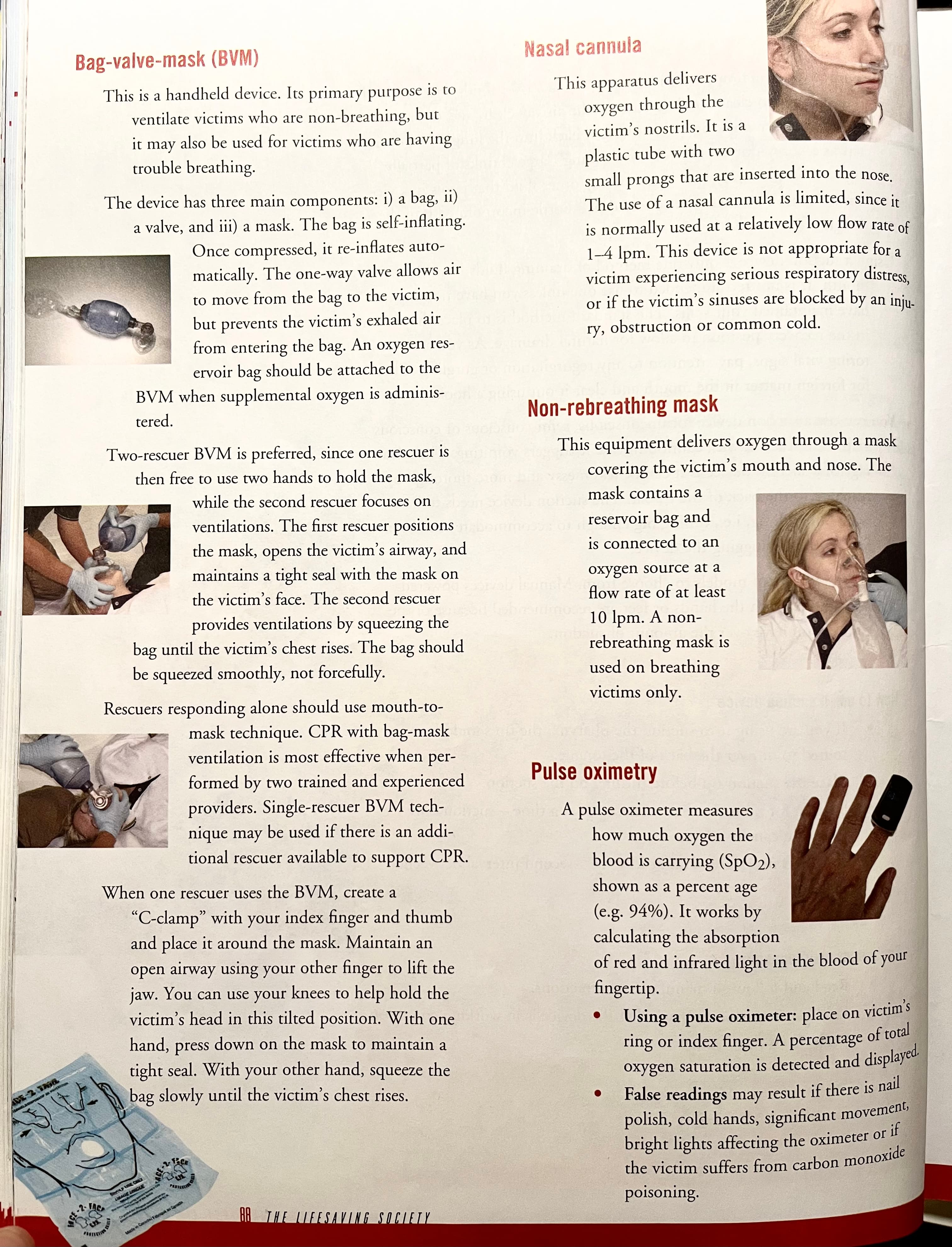
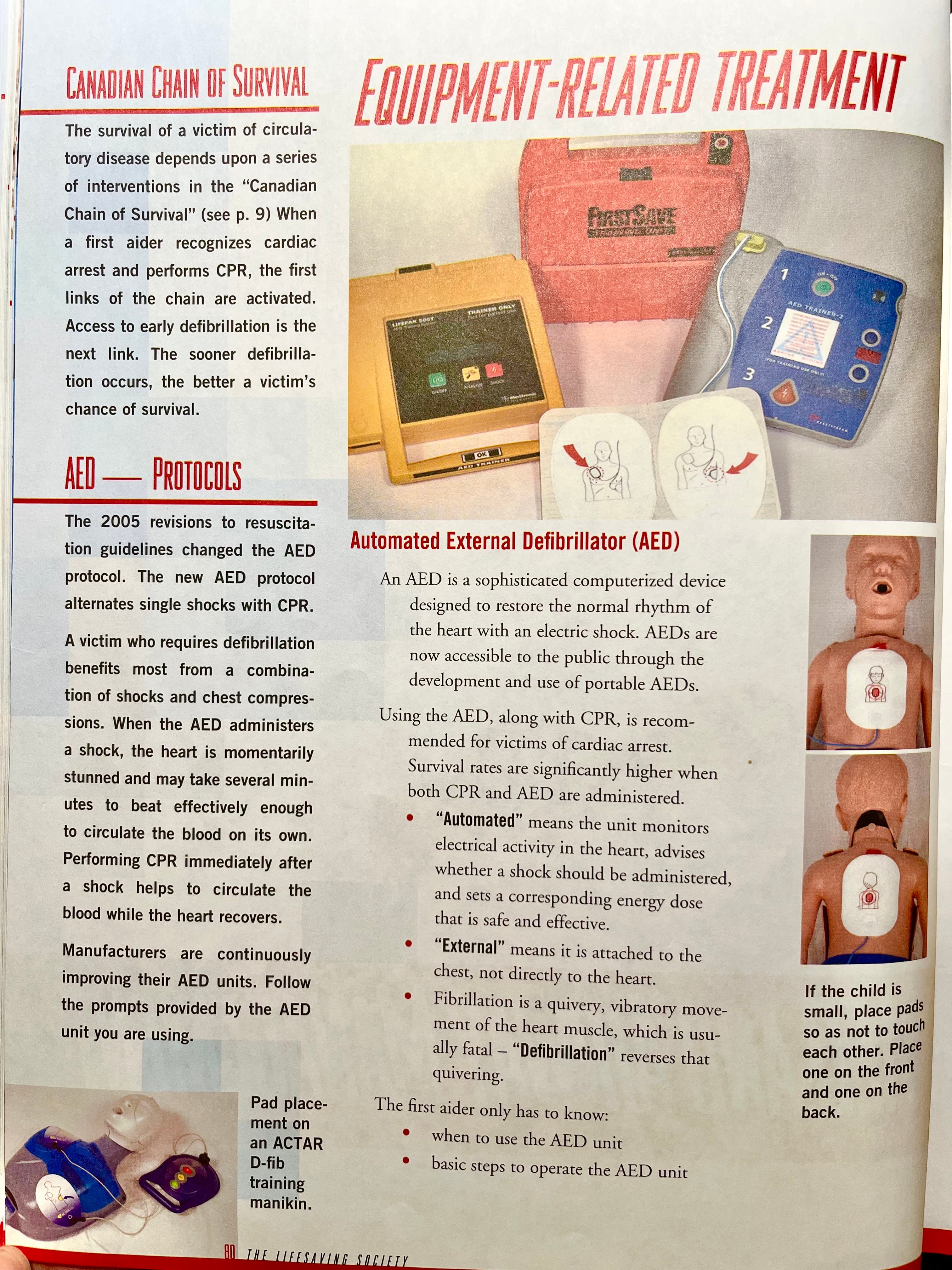
Equipment
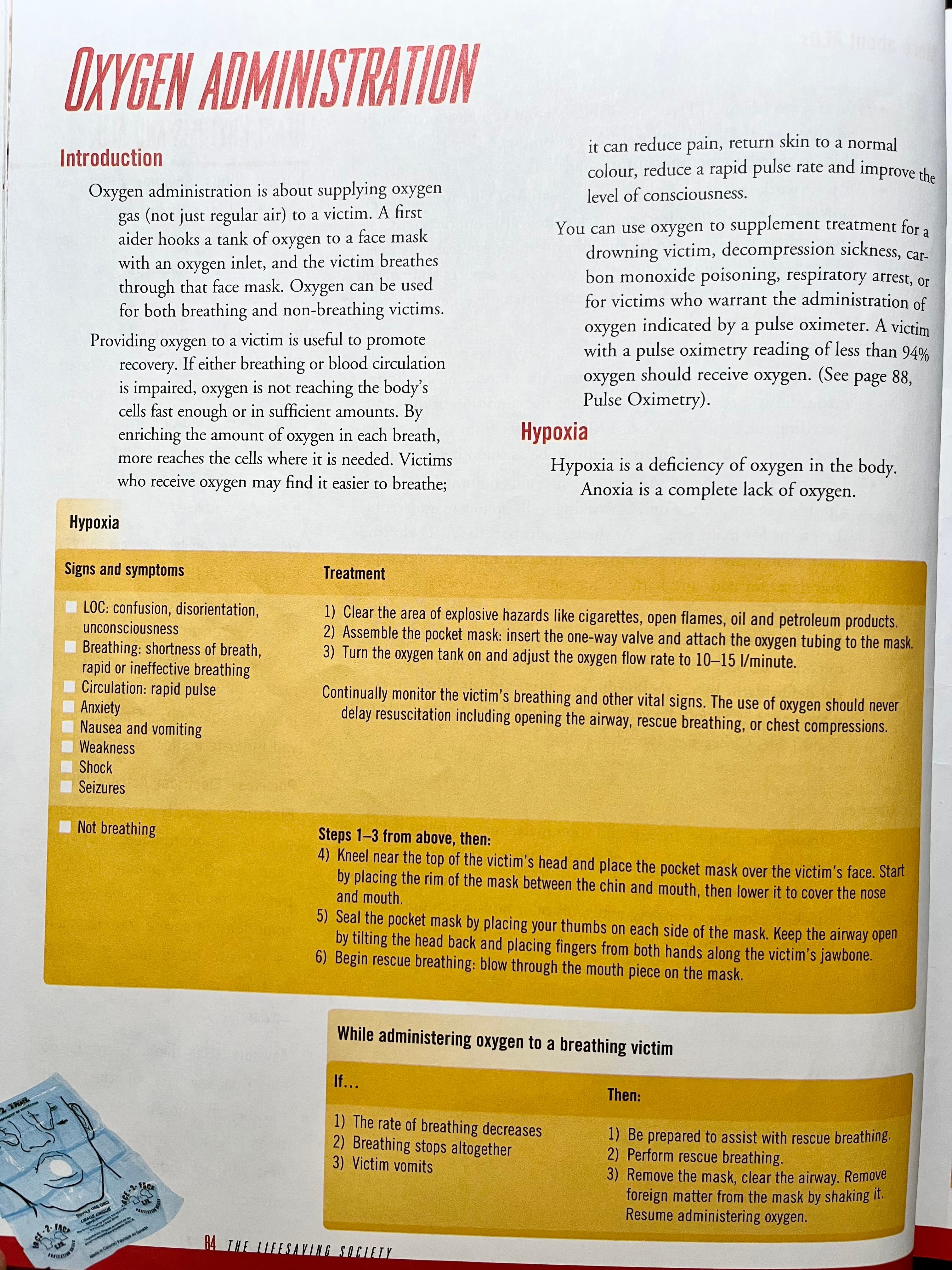
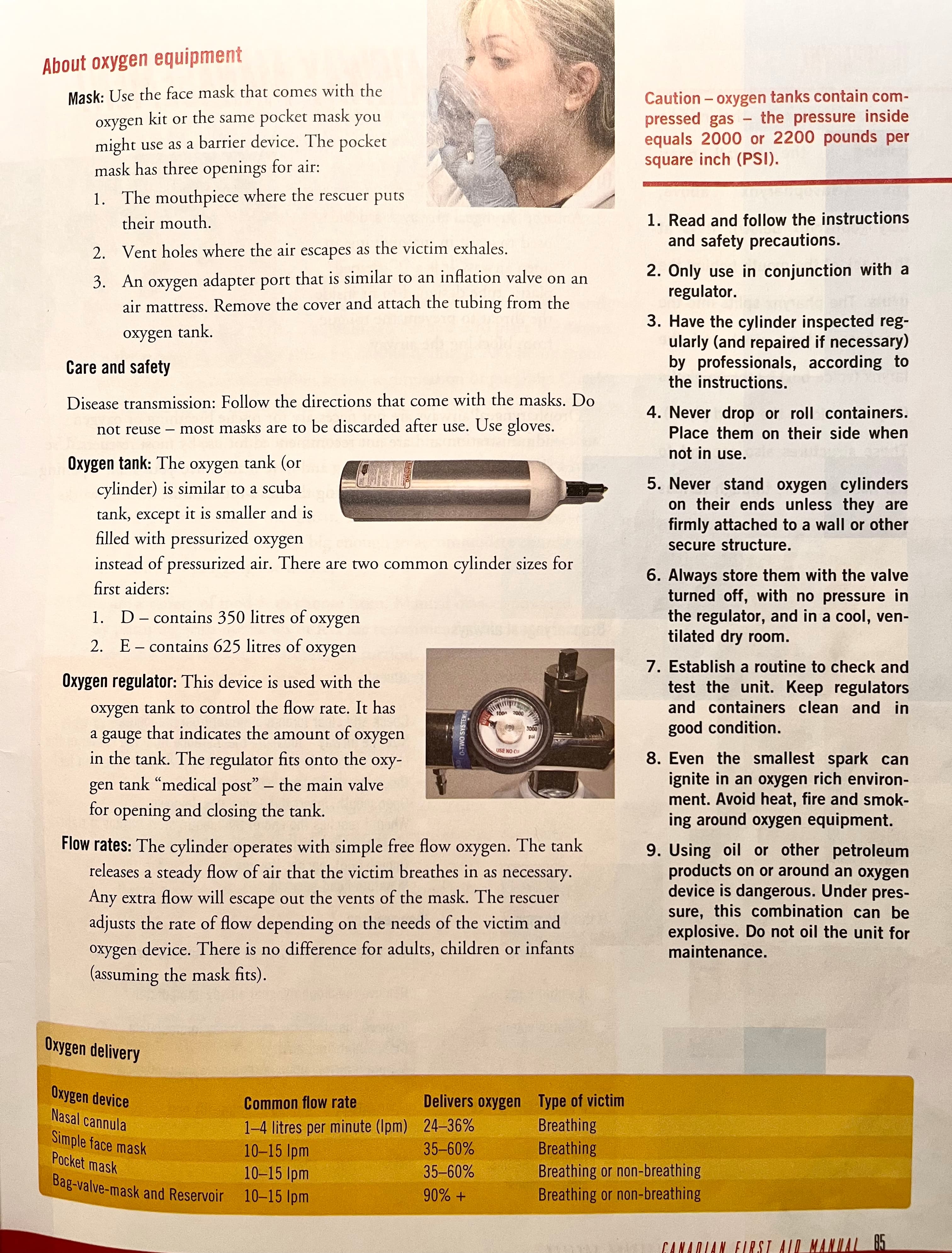
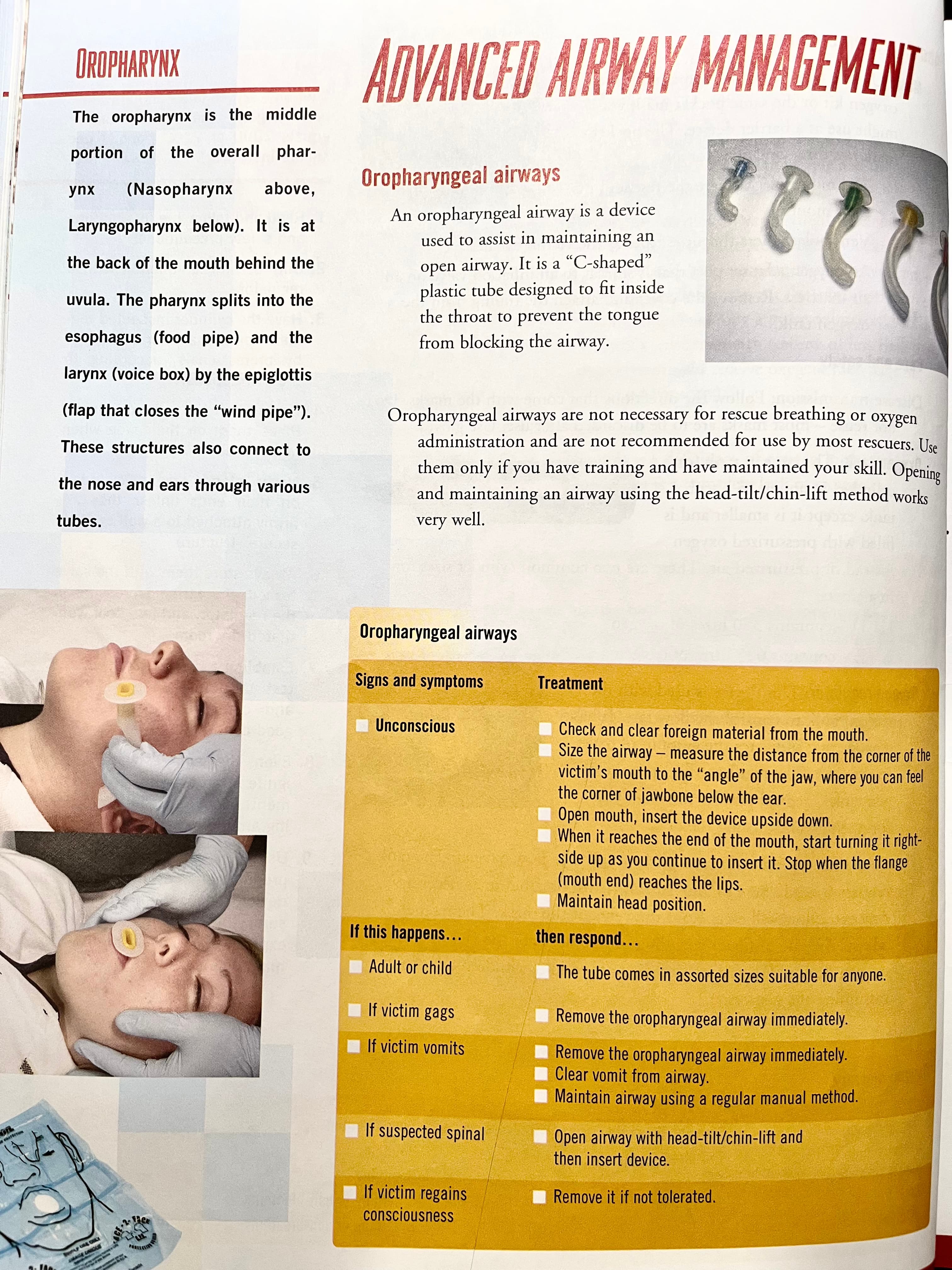
Oxygen administration